Robotic-Assisted Proximal Gastrectomy with a Laparoscopic-Assisted Double-Tract Reconstruction for Proximal Early Gastric Cancer
1Seoul National University Hospital
2Dana-Farber Cancer Institute
3Brigham and Women’s Hospital
Transcription
CHAPTER 1
My name is Dr. Do Joong Park, Seoul National University Hospital. I'm a gastric cancer surgeon. Today's case is a male, 70-year-old male. He already underwent endoscopic submucosal dissection for early gastric cancer. However, the final pathology proves incomplete ESD. So, we planned to perform laparoscopic proximal gastrectomy. Because this patient is an early cancer, we prefer proximal gastrectomy to total gastrectomy, because there are several benefits after proximal gastrectomy. So after proximal gastrectomy, we have some disadvantage of reflux esophagitis. However, recently after introducing double-tract reconstruction the reflux esophagitis is nearly the same as total gastrectomy. So, in Korea, the proximal gastrectomy double-tract reconstruction is increasing. So, let me show today's operation about laparoscopic proximal gastrectomy with a double-tract reconstruction.
CHAPTER 2
How do you plan your ports for your robotic approach, Dr. Park? We have a five ports, and this is a 5-mm, 8-mm, and this is a 12-mm for the assistant port. And these two are 8-mm. Is there a certain distance from the xiphoid or the umbilicus that you aim for? Actually, da Vinci Xi, might be 5-cm will be okay between trocars, ideally 10-cm. Okay. Needle, please. Grasper. One more, please. Gauze, please.
CHAPTER 3
Place the scope to the target anatomy. Then, press and hold the targeting button. Targeting complete. Stop the remaining arm. Oh, okay. Could you clean the vessel sealer?
CHAPTER 4
Okay. Chungyoon, please lift up the liver. And, is there any replaced artery? This one. Okay, let me see the…
I think this is not so big, and the tumor is located at the cardia, so might be this should be sacrificed, had better sacrifice, I think. Do you try to preserve certain accessory or replaced hepatic vessels when you have early versus advanced cancer? Usually in early cancer I preserve, but this patient has the tumor at cardia, so it is very close to the tumor. So, I think this should be sacrificed for the effective lymph node dissection. Large clip, please. And I think this is accessory left hepatic artery from left gastric artery, not replaced artery. So, even though I cut this, it'll be okay. One more, please. One more large clip. Position up, please. Okay, medium clip, please.
Is this Prolene that you use to hold the liver? Yes, right. This is a very convenient method. Chungyoon, this.
CHAPTER 5
And then, I want to make window, first omentum, greater omentum. So, I always do a partial omentectomy, in the middle of lymph node 14 area. Chungyoon, release and regrab the posterior. I detach all of the adhesions at posterior surface of the stomach for effective dissection. Could you clean the camera? Let's go. Chungyoon, please remove proximal part. Okay, up. Might be, this area is previous ESD area. Already there are the adhesions and some infiltration. So you want to avoid grabbing anywhere near there I guess for your? Yes, yes. Right. But, because this is not tumor itself, so no problem, but might be little difficult to grab the region itself. This is the dissection plane. Actually, this patient has had endoscopic submucosal dissection, but the T margin is positive, so the reason why we require gastrectomy is for lymph node dissection, not the resection of the region itself. This is the left gastroepiploic vessels. Please pull toward the GB. This is the left gastroepiploic vessels.
Okay, this is left gastroepiploic artery and vein. Large clip, please. And please grab more proximal part. Okay. Up, please. This patient has early cancer, so I just wanted to dissect only number 4sa and lymph node 2. Do not dissect around the splenic hilum.
This is the short gastric artery and... Large clip, please. Chungyoon, this one, please. Okay. Usually, I want all short gastric vessels cut. I've also noticed that some surgeons will use the harmonic rather than the vessel seal on the robot. I get that the vessel seal has more degrees of freedom, but are there times that you prefer the harmonic for this operation? Yes, but I believe vessel sealer has more good sealing power. So like this, vessel sealer is good for sealing for short gastric vessels. Sometimes harmonic, it's not enough and makes some bleeding. Chungyoon, pull up this one.
I want to detach all of the adhesions between posterior wall of the stomach and pancreas here. For transection of distal stomach, we should detach all adhesions here. Another gauze - release. And let's move to the lesser curvature side.
This is a branch from left gastric artery, and, this branches from right gastric artery, so this point is the landmark. I see. This lymph node 3a and this lymph node is 3b. Push down here. Is this also the landmark of where you plan to divide the stomach? Yes, right, but it depends on the location of the tumor. If the location of tumor is at GE junction and cardia, I can preserve more. But if high body, yes, this line. I preserve lymph node 3b and I dissect all lymph node 3a. Sometimes we can use indocyanine green, ICG, for lymph node mapping, but it's okay without ICG. And compared to a total gastrectomy, so you would preserve the station 6 lymph nodes here and you wouldn't go after them? During total gastrectomy, we should remove all lymph node 3. But the proximal gastrectomy, we remove only lymph node 3a from left gastric artery. This is lymph node 3a and this is lymph node 3b. We resect all lymph node 3a here. But you won't go to station 5 or 6 to sweep lymph nodes up? Lymph node 5 - we preserve lymph node 5 during proximal gastrectomy also. However, total gastrectomy, resect all lymph node 5 also. And press down here also. In obese patients, this plane is a little deep and difficult to divide, but... Chungyoon, could you show the posterior wall like this?
CHAPTER 6
Might be the tumor was here, and this is the landmark between left gastric branch and right gastric branches. So the transection line might be from this, vertically here. We can adjust the transection line if the tumor is located at the greater curvature, might be the lower transection margin, but this patient at cardia, so I can preserve more greater curvature. Anyway, it depends on the tumor location, and okay, transection here will be enough. And then we clear the greater curvature side. Chungyoon, okay, here. Large clip, please. Vessel Sealer. The laser. Chungyoon, insert the stapler. We will transect the stomach. What kind of stapler do you like to use to transect the stomach? I use Signia and Echelon, sometimes both. Recent staplers are very good. Okay, open. And, okay. Wait, wait. Down, please. Down. Please bend to left side. Okay, I will adjust the lesser curvature. Okay. Close. Fire, please. Hmm. Okay, one more, please. Okay, open, and bent. Okay, now wait. I will help you. Wait. Oh, wait, wait. Ah, okay. Okay, close. Fire. Good job.
CHAPTER 7
Please insert suction. Suction here, caudate lobe, and press down the... Okay, the large one, suction, I'm gonna help on the large one. This is lymph node 8a, and this is the common hepatic artery. Suction... Press down here. Press down here.
This is left gastric vein, coronary vein - suction. So a medium clip. Suction. Suction. Okay. Press down here. This is the left gastric artery. Large clip. So one more. Press down the pancreas, here. Let's just see the whole - this is the common hepatic and left gastric and splenic here. Gauze out, please. Gauze out. Gauze out. New gauze. One more gauze. Big wrap here. This one, please.
CHAPTER 8
Oh, okay, release. Release. Press down here on lesser curvature side. You're just clearing out the abdominal portion of the esophagus and you're looking for the vagus? Yes. Vagus nerve. I already cut the vagus nerve at this point and I want to clear more around the esophagus. Okay. Okay. Okay.
CHAPTER 9
And again.
CHAPTER 10
This is an auto purse-string device? Yeah, laparoscopic purse-string clamp. Okay. I'll help you. Oh, okay. Here. Camera.
Dr. Park, you prefer simple staple. What about linear staple? Oh yes, it's okay. Linear staple is also another good option. When I do totally robotic surgery, I do linear stapler method. Do you find any difference between two methods? Not so big difference. It's the surgeon's preference. I have several videos of a totally robotic surgery with the linear stapler. Yeah, yes. Sure. If the region, the anastomosis will be very high, we should do linear stapler method.
CHAPTER 11
Okay. Frozen section? Yes, yes.
CHAPTER 12
Just see the... Okay. Okay. Okay. Nice stitching. Yeah! So... This is proximal. Should we send a margin from the mucosa on the proximal and distal side? Yes, sure. This is proximal. Please.
CHAPTER 13
Usually we send the full-thickness margin, not only mucosa, but also the whole thickness.
CHAPTER 14
Release the dissector. Dissector. Chungyoon... Release. Okay. Because the lumen was open, so we avoid contamination before anastomosis. How far out do you like to divide the jejunum? Usually 15 cm from Treitz, but sometimes 20. Okay, release. Okay.
Okay. Marking pen. This is 15 cm from Treitz, and I will cut at this point and 15 cm below. This will be a gastrojejunostomy. And 20 cm below, jejunojejunostomy.
Cut, please. Okay. Fire. Stapler. Pull this small bowel. Okay. And... Okay. Tie. Yeah, yeah. Cut. Okay.
Do you always close the Petersen's defect, Professor Park? Oh, we don't repair Petersen's defect, only mesenteric defect, because the anastomosis is a little high, so Petersen's is not so frequent. Mosquito. What are you using for the swab? I think it's chlorhexidine. This one please. Mosquito. Stapler. Tie. Ooh!
Stapler. You tie. Surgical tie... Cut. Okay. Open. Ah, okay, good. Ready to see the final view?
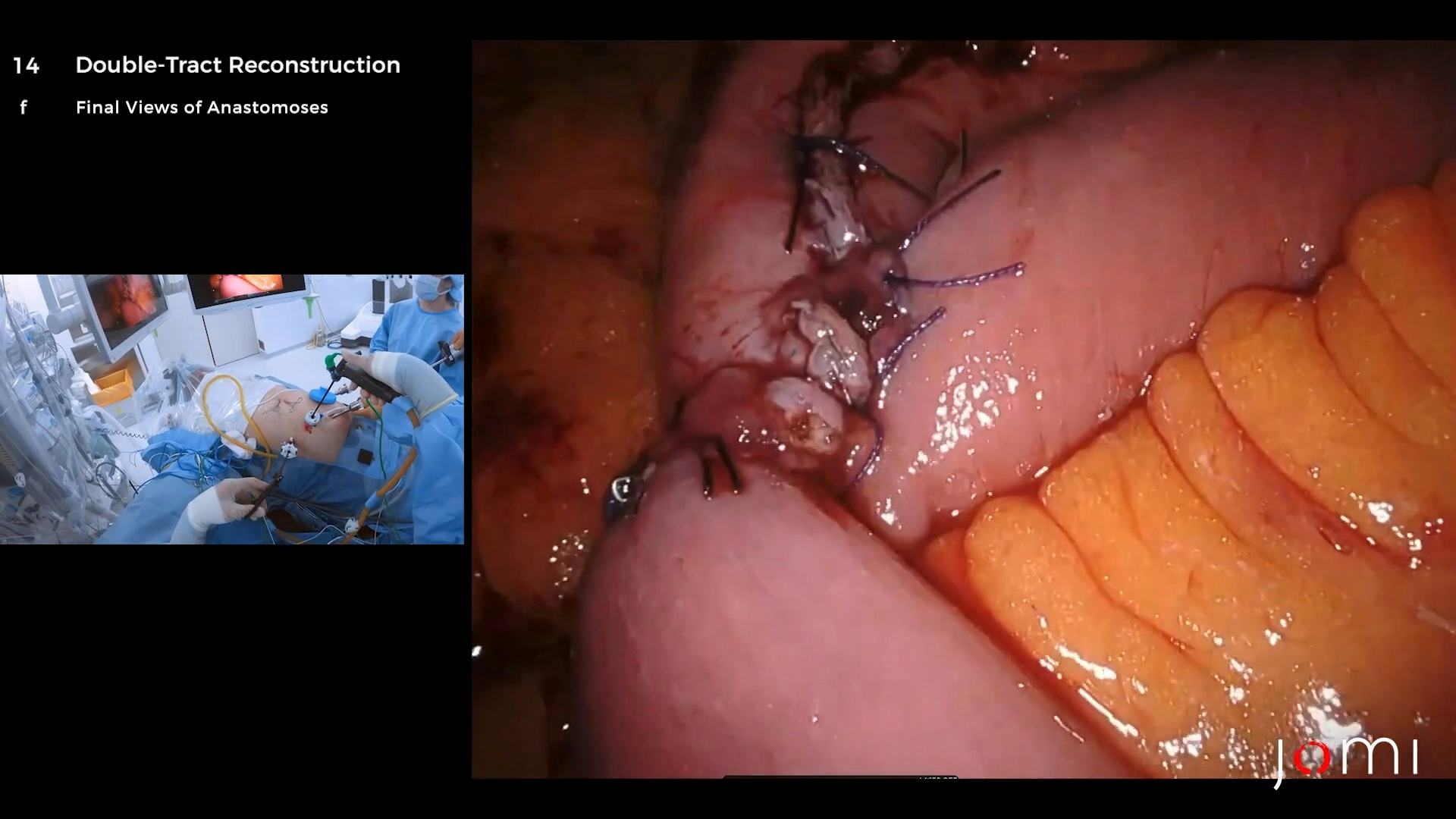
This is the final view of anastomosis. This is a esophagojejunostomy and 10 cm below, gastrojejunostomy here, gastrojejunostomy. And 20 cm below, jejunojejunostomy. What portion of the food goes to... Yes, right. According to our retrospective study, on radionuclide emptying study, 60% of food passes through the duodenum, then to the stomach, and the other 40% passes through directly jejunum.
And I always fix, I always fix the remnant stomach to here, intrapyloric some connective tissue, because some patients complain of pain, postoperative pain. This is somewhat redundant, so I will pick here. Are there any other functional advantages to proximal gastrectomy over total or any trials that... Yes, we have a very famous class trial, class 5, 05. The final result were published in JAMA Open this March. So according to our study, some vitamin B12 preservation and some quality-of-life benefit we demonstrate. So I will send the relevant article to you. Medium clip. Is there also an advantage for hemoglobin? Actually, partially, but we didn't demonstrate hemoglobin change for two years, but I believe after two years, might be a benefit in proximal gastrectomy. According to our retrospective study, there was a benefit of proximal gastrectomy in terms of hemoglobin also. So anyway, I will send the package of our trial later. Okay, so we finished our anastomoses, and we can do gastrojejunostomy anterior wall and create a curvature. But I prefer the posterior wall of the stomach. And the length is also based on the surgeon's preference. But the longer, the better of reducing the esophageal reflux. But if the length is too long, it is difficult to apply screening endoscopy, surveillance endoscopy. Okay.
CHAPTER 15
[No dialogue.]
CHAPTER 16
[No dialogue.]
CHAPTER 17
[No dialogue.]
CHAPTER 18
I finished the laparoscopic proximal gastrectomy with a double-tract reconstruction successfully, and for this patient, two days after proximal gastrectomy, sips of water begins, and followed by semi-fluid diet and semi-blended diet and he will discharge, it might be on postoperative 7 days, I expect. And I expect this patient has advantage of vitamin preservation, of vitamin B12 level, and he will not need to get any intramuscular vitamin B12 supplement for a life-long time. And he might have some advantage of less hemoglobin change and less weight loss. And there are some GI hormones produced by the distal stomach, so I believe there are some advantage after proximal gastrectomy.