Robotic-Assisted Laparoscopic Left Donor Nephrectomy for Living Kidney Donation
Massachusetts General Hospital
Transcription
CHAPTER 1
I am Leigh Anne Dageforde, and today we're gonna show you the steps of a robotic-assisted donor nephrectomy for someone who wants to donate a kidney to a recipient. The key steps of the procedure really start with the positioning where we are moving the patient to the lateral position and we wanna make sure that all the appropriate points are padded. So we really are careful about padding their arms, making sure the neck is straight so there's no strain and padding the legs as well. After the patient is in the position, we make an incision down low where a C-section scar would be or a Pfannenstiel incision and it's somewhere between six and a half to eight centimeters depending on the size of the kidney that we expect to come out. We then use three other port sites that go laterally and those are where the robotic instruments and camera are docked. So after we make all of our incisions, we bring the robot in, we dock the robot and put in the instruments and the camera. And from there we actually then move on to the next step, which is to unscrub and sit at the robotic console. Once we're at the console, we do the first step, which is to rotate the colon forward, so we rotate away everything that's in front of the kidneys. Since the kidneys in the back are retroperitoneum, we move the colon forward, we identify the ureter as our next step, follow the ureter more up towards the kidney. We also rotate the colon away. We also rotate the spleen forward along with the tail of the pancreas so that we're able to identify the hilum of the kidney. We follow the renal vein and identify the gonadal vein and the adrenal vein on the left side since this is a left nephrectomy and we divide those and then we identify the artery. From there, we mobilize the kidney, which means we separate the kidney from the adrenal gland, we mobilize the superior end of the kidney, and then identify the artery and the vein from the posterior side of the kidney. And sometimes there, you see a lumbar vein and so that's often divided so that we can safely eventually divide the vein and the artery. After everything is cleaned, we divide the ureter by making two clips on the distal portion and then we cut the ureter. At this institution, we've decided to remove the kidneys with hand assist, although there's several different options that people use, but I scrub back in and then we use a GIA stapler with a 30 load to divide the artery and the vein. And then we remove the kidney through the low Pfannenstiel incision. Once the kidney is removed, the staple lines are cut and then there's a flush through the artery and the vein and we make sure that the kidney is flushed with the preservative solution and stored on ice. While that's taking place, the assistant's major role is to make sure that there's no intraperitoneal bleeding in the donor. After that I do a TAP block and so I place local numbing medicine along the lateral edge of the peritoneum. We also put local in the large Pfannenstiel incision and then three other port sites. And then we close everything in multiple layers. And the top layer, I use surgical glue.
CHAPTER 2
When we position the patient, we position them on their side with the side where the kidney's being removed as the side that's up and then they're laying in the lateral position. Obviously we wanna be careful to pad all the pressure points and to make sure that the arms are well padded and positioned appropriately. We also work with anesthesia to make sure that the neck is straight and then we make sure that the extremities, the knees are also padded and positioned well. I do warn the patients in advance that they could wake up with a funny bone feeling 'cause we're of course positioning them while they're asleep so they can't tell us if something feels unusual or it's pinching, but it's very uncommon to have that issue. And then before turning the patient lateral, we mark a finger breadth above the pubic bone and I make a about a six-and-a-half or seven-centimeter-long incision because we take the kidney out with a hand assist. And so that's for the GelPort. But obviously I think depending on the site, some people use a bag and maybe make a smaller or if their hand is larger, the kidney's larger, slightly larger incision. But because the abdomen shifts, we always mark them once they're on their back. We also have a catheter in place, a Foley, obviously to decompress the bladder as we're making a Pfannenstiel incision so we don't get into the bladder.
CHAPTER 3
Okay. All righty. Great. We'll take a knife. Insert here or there? Do you mind raising the bed up a little bit? Sure. So again, this is a Pfannenstiel incision. It's about a finger breadth above the pubic bone. Great. Is that good? Yes. Thank you. In women that have had C-sections were often able to reuse the same site 'cause it's essentially in the same location. Can I have a Weitlander? DeBakeys, thank you. Schnidt. And a Rich, please. And a lap. Great. A little bit more. All right, we're gonna make an incision here. So now we've cleaned off down to the fascia. So we're gonna just make an, open the fascia bits down to where we see the muscle. Right, I'm gonna open it the other direction as well. It is always easier to go down than up, as gravity works with you, I think you can just make a cut and open it a little. Great. All right. A little bit more there. Okay. We'll take some Kocher's. Now we're gonna raise flaps so that there's enough size to take the kidney out. So this is over the rectus, and we're gonna come in this kind of clear area between the muscle and the fascia. After you open the skin in the fascia, this really becomes the limiting size factor. So you have to raise a big enough flap that the vertical incision is enough for the kidney to come out. Great. So you're gonna raise flaps both up and down. Okay, great. I'll take the Rich back. We're gonna open the peritoneum here. So we're gonna go in the midline, sort of the space between the rectus muscles. I'll hold that. Gonna open that a bit more and go ahead and open that. Just grab... Gonna pick up across from me there. Yep. Can I have some Metz for us. Maybe we're in. Great. You can go ahead and take the... Again, we're gonna open the peritoneum, superiorly and inferiorly. It's important here to be careful that you're not pulling up the bladder 'cause you're so low. So between the Foley decompressing it and then just being cognizant of where you are, it's just important not to accidentally pull that up and you have one more layer there. Do you have some Metz for us? Okay. Yep. Alrighty. I think so. It's got some... Maybe. All right. Open that a little bit more. I can't quite see. I'm gonna come right back up here. I'm gonna open that a little bit more. All right. So no adhesions, which is nice. We'll take the GelPort. All right. And it's important to make sure that there's no bowel or omentum trapped under the edge of the port here 'cause we're gonna roll it down and pull it up to the abdominal wall. We don't want it to be compressed or under pressure. All right. Very good. All right, we're gonna insufflate. Are you ready? Our donors are often very healthy and so sometimes they tend to get bradycardic with insufflation. So it's always important to check with your anesthesiology team and make sure that they're ready for insufflation. Seems that the healthier they are, the more likely that is to happen. So we're in constant communication. And then we use the GelPort and we use an assist 12 port that will actually stay in for the PA with the robot that's gonna be at the bedside. So this will be an assist port throughout the case. Yeah. Okay. All right. Do you have a marking pen? So we're gonna look to where the kidney is and go about two finger breadths from all the bony structures. So about two down from the rib cage here. And then we'd have to go about 10 centimeters. So about a finger breadth, that was about there, maybe a little... Okay. And then about 10 centimeters apart. It looks a little low to be honest. Maybe we'll go a little bit higher. And then 10 centimeters down and also about two centimeters from any bony prominence down here. We put this one up a little bit higher, recognizing that we also have to be able to reach to rotate the ureter. It's kind of short from here to there. Okay, we'll take a knife. Okay. All right. On the robot porch, you want the one line on the inside and the line on the outside depending on how thick their abdominal wall is. But what you don't wanna see is the thick line. I think the port is open. There you go. We'll take another line. So again, we mentioned this is what's hidden in the abdominal wall. So you don't wanna see this thick line on the inside or the outside. Great. It'd be easier to come up from the top. So again, two centimeters from any bony prominence, which is about two finger breaths and then 10 centimeters apart, which is about a hand width. So we choose to just use three ports even though the robot has four arms for our donor cases. 'Cause there's actual... Often the donors are... There's not a lot of room to fit the fourth port. So, all right. Great. So now we're gonna have them drive the robot in.
CHAPTER 4
I'm gonna just check my hand here. Which one you want it on? Here. Hey, Cole, does the bed height go down at all? I'm gonna just... Drive the laser line to the endoscope port. You wanna make sure you can... It's stuck though. Yeah. You okay? Yeah. Which way did you want this? I wanna add... Like at the bottom now. So we drive the robot in with the target of this green X mark being over our middle port. This is gonna be our camera port. As I mentioned, even though there's four arms, we only use three. And so we put our upper arm off to the side and then dock our remaining arms. I'll take a camera cloth and the Q-tip, please. We're gonna start by docking the middle port, which is the one that the camera goes in. Install the endoscope for targeting. So targeting for the robot... Press and hold to target anatomy, then press and hold the targeting button. It's gonna define where the arms rotate. And since we have to work all the way to the pelvis for the ureter and all the way up towards the spleen, we sort of pick a place that's in the middle to do our targeting. So, this is roughly estimating the lower pole of the kidney there. Targeting complete. We dock the remaining arms. And I use a hook in the right hand, although some people use scissors. And then we use a fenestrated bipolar in the upper. And the nice thing about the robot is that both are able to have heat. I want to carefully follow the instruments in. Great. All right. Okay.
CHAPTER 5
So the first step is going to be to rotate the colon off the abdominal wall. One thing that's important in this process is not to go behind the kidney just yet as that will rotate the kidney down and the retraction of the kidney back against the abdominal wall is nice so that we're able to work around the hilum. So picking a point that's not necessarily going behind the kidney quite yet.
CHAPTER 6
So we're gonna look for the ureter. There's the ureter here. You can see it vermiculating. Mobilize a little bit more of this forward. Again, we're wanting to stay out of the mesentery of the colon. So, we've rotated the colon forward. And in general you take the ureter to about the level of the iliac. One thing to be careful about is stripping the ureter. So we want to give the recipient surgeon enough fat around the ureter that it is not... Stripped of its blood supply. So there's a fine balance between taking too much fat and then not quite enough. And so we'll try to take a little bit of fat... Up with the up with the ureter. Just careful dissection. You can see some of the vessels that go along with the ureter. So we're gonna be careful with those. And include some of them in what we take. And then I am just gently holding the tissue around the ureter, but I don't want to grab the ureter with my left hand 'cause it has kind of a tight grip strength. So we wanna be careful not to crush the tissue of the ureter. And here you can see the assistant port has the suction, which is very helpful since we don't have that additional fourth arm. And I'm gonna encircle the ureter with a vessel loop to allow for some gentle retraction without picking up the ureter. Again, this comes in through the assist port. Thank you. This is nice for retraction. One thing to be careful of and to note with the robot is that you don't have tactile feedback. And so it's really important not to pull too aggressively on the vessel loop. And one way that you can tell is when there's blanching of the tissue. And that's one way to tell how strongly you're pulling. Great. Thank you. And we're just gently doing some retraction and elevating the ureter here. And as I mentioned, we're gonna go down as far as the iliac, but we may come back and do some of that with our vessel sealer. So, let's move our attention on up here. Thank you. Great. Thanks. Again, the importance of having a great assistant at the bedside. Another thing to notice is that the heat spreads and so some small taps instead of just laying on the foot pedal for the burn is helpful.
CHAPTER 7
All right, so now we're gonna work to continue to rotate the rest of the colon away here and get into the retroperitoneum. Everybody's kidney has a little bit of padding on it, but each patient is different in how much they have. And we'll work to mobilize the spleen as well, which we wanna rotate away. Do we have an OG tube in? And could you put a dissection, please? It's good to have the OG tube dissection 'cause the stomach can come up behind the spleen. So we always have our anesthesia team decompress the stomach for us. Obviously we wanna be cautious about the spleen and not retracting too aggressively in a way that could tear or damage the spleen. Again, we're just working to get into the correct plane here where we're working in the retroperitoneal space. Each kidney has a different degree of padding, fat - Gerota's fascia. I can see our ureter back here. So, carefully divide some of this in between. So here's kidney, finally, sort of under some of this padding. All right, just working around some of the additional fat here. Just looking to carefully rotate some of the fat away so that we can see the hilum and the hilar structures carefully. Again, we're looking for hilar structures. There's inferior pole. Coming up. I think there's renal vein. Certainly rotating this off up here will be helpful. Quite a bit of fat around the kidney, so taking some time to mobilize that away from the kidney. I also see that it's a large kidney, so it's going quite far back towards the spleen here. So some edema of the tissues that you can see here. Also in this area, we think about the adrenal gland, which might be hard to see today in him. So there we can see the renal vein.
CHAPTER 8
We don't want to do the dissection right in the hilum because there's often branches. So, you wanna work a little bit more away from the hilum. And each case is different with how much fat there is to work through. So, we'd like to see the gonadal vein and the ureter here, in this area. So we'll do a little bit more dissection and see if we can identify them. Just trying to find a plane here through the fat. Again, the vein. See the edge of the peritoneum there. I think perhaps we'll look here. From this side we can see the gonadal vein. So there's ureter from this side, you can see down in there. So now we're just going to connect by removing this that's in front, dividing some of the extra fat. All right, gonna look in the space here. You can see the ureter again there. Now we're looking for the gonadal vein. So a little bit more to take here to get this connected. Here's our gonadal vein, which we can see here. Little bit of this. Again, we're gonna sweep the ureter up. A little added fat with it. And it will be helpful to find the ureter and the gonadal here as we're coming into our renal vein. All right, let me look under where you are. Okay, so now then, still looking here for the gonadal. A little bit more... Now hold up there for a minute, Jess. Yep, thanks. So there's the gonadal vein, which we do have to divide on the left side because it goes into the renal vein. If you were doing a right, usually it goes into the cava, so it's not something you have to divide on the right kidneys. We're gonna clean it off and then use the vessel sealer device to divide it after we get it cleaned off. All right, we'll take a moment while we're here and look for the adrenal, which is on the other side of the renal vein. And again, on the right, you don't have to take it. Do you mind suctioning right there for me? You can see hints of what may be the artery being pulsatile there. Lots of extra padding in this particular patient. All right, now let's go ahead and take the vessel sealer. Maybe we can clean the hook while it's out. And then do you wanna do a camera clean too?
Great, thank you. All right. I take this with three burns, so... Away from the vein so you don't risk burning the vein.
All right, so we've taken the gonadal vein. So next we look for the adrenal. This puts some added challenge here due to the fat. So often the adrenal would be down here. I think there it is. It's just added difficulty with the extra fat. I think you can get any lower here on this fat. Yep. Great. That's perfect. All right. Thank you. There's our adrenal vein. Just trying to dissect carefully to get it circumferential. And the vessel sealer only cuts to the white line, so... It's important to be around it. Just a little bit more to get all the way across. All right. Okay.
CHAPTER 9
Right. So the artery, certainly we can see a pulse back in here. Sometimes there are small branches off the vein along the edge here that need to be taken to look carefully with that. It's often helpful if we can identify the artery before we mobilize the adrenal to ensure that we know the path of the artery. Okay, the artery's starting to come up. Can see the artery sort of coming into view there. Right in there. So, we have some that we could take here off of the front of the artery. You just have to be careful, the edges of the vessel sealer also get hot, so you don't want to have those up against the artery or vein.
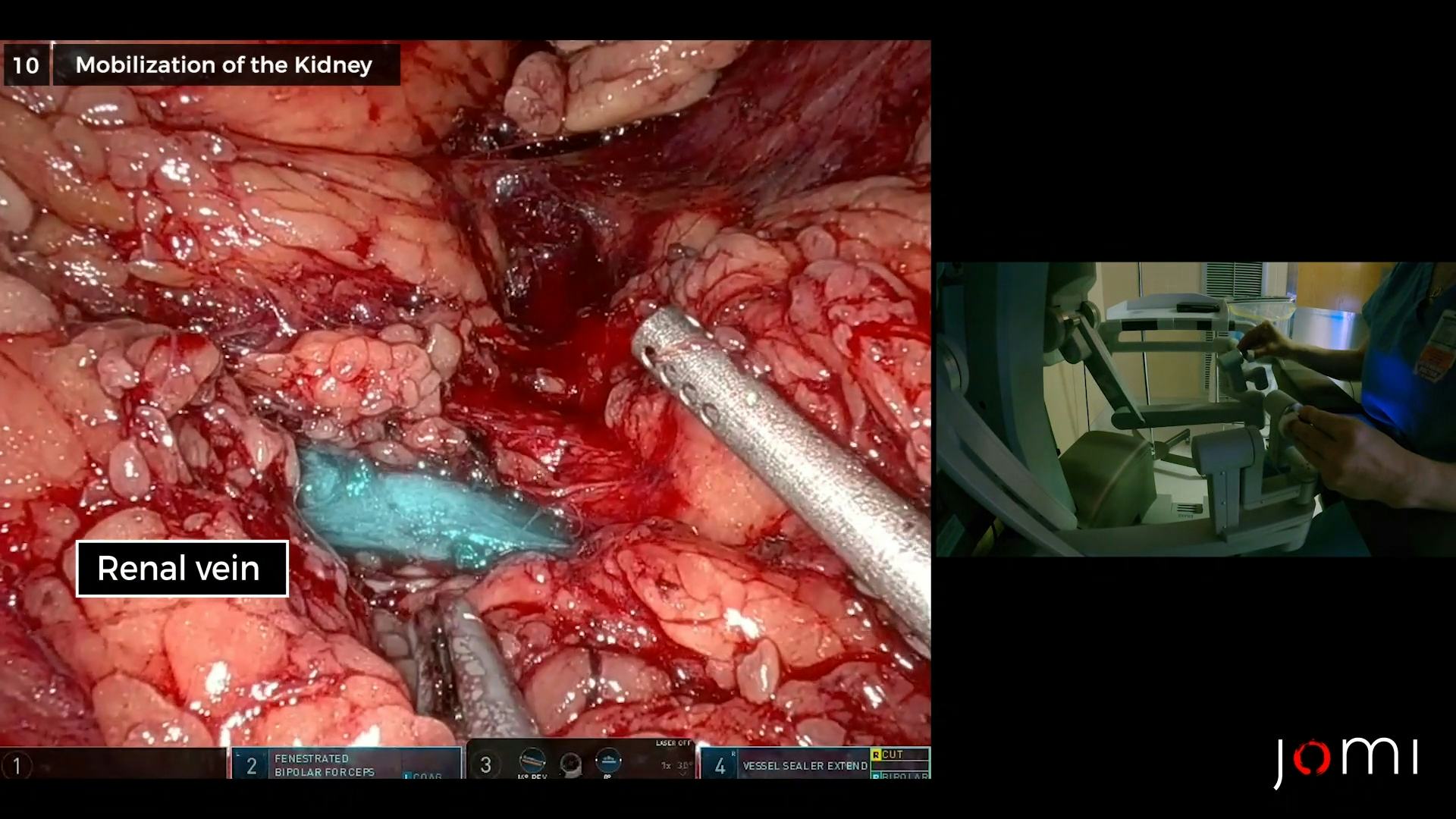
CHAPTER 10
And once we know where the artery is, we can start to take some of the divide between the kidney and the adrenal gland, trying to be cautious of any potential upper pole artery branch. How are they doing in the recipient room? Okay, thanks. I'm gonna try to separate the kidney from the adrenal here. And careful not to take any branches, times when there's sticky fat on the kidney, it's tricky. And just dividing some small branches here from the vein. Another small branch off of the vein as we mentioned. I am trying to... All right, just looking here as we mobilize the upper pole of the kidney, quite a bit of sticky fat around the kidney here, so... So we're gonna just move on to mobilize the kidney a bit here and see if we can get some better visualization of the vessels. Now that we know where they are, we will send this kidney with some fat on it for them to do on the back table of the recipient, since it's fairly stuck to the capsule. Dissecting out the ureter here. We're sweeping the ureter up here, dividing between the ureter and the vein. We get closer, there's often lumbars, so we'll want to watch for those. You can see the nice length on the renal vein, which is very helpful to the recipient surgeon. Okay, so we're gonna take this ureter up. So posterior side of the kidney here. So we're gonna work to mobilize. The recipient surgeons also like less fat, but sometimes when this fat is very adherent to the kidney, it's better to send it with the fat so you don't get into the capsule trying to take the fat off. Okay. So again, we're just mobilizing the kidney here. There's a lot of additional fat, which is adding to some of this. And coming up from behind, we'll start to see the hilar structures from the posterior aspect of the kidney. It just has an added layer of some fat here. There's slime on the camera. You wanna fix that for me. So again. Mobilizing the superior pole of the kidney. I think you can hold the kidney back for me. Thanks. You can see a small branch there to the upper pole, so we're gonna stay out of that. All right.
I think there's a lumbar vein in the back there. Nice. Maybe we'll see that from the back. We can see the vein and the lumbar vein there. We should be able to also see our artery from behind. We've divided the lumbar vein. So now we're gonna look for the artery from the back. In the midst of some fat. It's a vein, I think that's wrapped on the back of the artery there. The artery and this little vein that I think we'll have to take so we can get between them to divide them. You can see the vein. And here's the posterior part of the artery. Just have a bit more to clean up before we can divide. Stapler. I feel like we're losing insufflation again. I don't know. Okay. Can you suction down in here? Is he totally paralyzed? Yes. Okay. I think there's a little... Why don't you go ahead and hang the flush and give 12.5 grams of mannitol, please. Yes, please. 12.5 grams. We can open the two stapler loads. You can tell Dr. Elias we're ready. Mind holding the kidney back for me? All right. We just wanted to make sure we're circumferentially around the artery, which we are. And the vein. And completely free from all sides, which I think we are. Okay.
CHAPTER 11
All right. We will take the ureter here. So we're gonna go distal, and we're gonna clip through the assist port. I can also clip through the... Yep. All right.
CHAPTER 12
We are gonna have to upsize the GelPort, I think. We're gonna have to... Oh, to get it out? Yeah. Thanks. So we upsize this lower port to a 12 so that the stapler fits. You have a knife.
CHAPTER 13
Some people take these out with a bag, some people stay with the robot to staple. We've selected to staple through our port here with a handheld GIA stapler. Is it free from the back? Let's look again. I'm gonna make sure our artery and vein are totally free. We can see them. Do you have a Maryland grasper? All right, we'll take the stapler. I think you're gonna have to suction so I can see to the staple. Gonna always make sure the ureter up and away. This. Cross clamp. All right, you also don't wanna catch the artery and restaple it in the vein. So you hold the artery back. We're gonna staple the vein. I relax the kidney a little bit so that I'm not pulling up while I staple. All right.
CHAPTER 14
Can I have more ice? Here. Ice. You wanna go ahead, you wanna check on the donor or? Yep. Looks nicely flushed. Yeah. Okay. All right. Thanks. Can I have some clips, please? Can you open a 10-millimeter clip applier. All right. So we're just checking the artery and the vein stump there where we've stapled to make sure there's hemostasis. Yep. Thanks. Thank you. My clipping's making it... There's something up here that's bleeding. There seems to be a lot of rundown with the left. Think this is all disconnected at the moment. Take it out. Okay. Can I have another lap? There's fat in this one. Okay. Maybe. All right. We'll have the local. Thanks. All right.
We just do a version of a TAP block on our own. Find the preperitoneal space and inject some local to provide longer-lasting pain relief. I put about 15 in laterally. All right. I'll use the rest of that around the incisions. Look up here, again. Looks better. Surgiflo? Yep. Do you have Surgiflo? I think it's okay. Yeah. All right. Thanks. Thanks. Okay. And we will close this port site.
CHAPTER 15
Does everything look hemostatic down there? Yep. Okay. Great. There you go. All right, just closing this port site because it's below the belly button and there's a risk of hernia. All right. That feels good. I'm gonna look one more time. Put the colon back if I can. Okay. I'm gonna watch this one. Okay. Take yours out. All right. We'll take a Valsalva if you would. Okay. That's good. Thank you. Just trying to get all the air out to reduce the pain in the shoulders. The referred pain from air trapped into the diaphragm. I'll have a lap. Okay. We'll have the overhead lights on. Can you raise the table, please? I'll take a Weitlander. All right, looks good. Thank you. Two snaps, please. So first we're gonna close the peritoneum. Thank you. And one more lap, please. And a Rich and a Vicryl. All right. Oops. Okay. Just gonna close the peritoneum first with a Vicryl. Scissors, please. Okay. Just making sure there's no bowel or omentum caught up. Some scissors, please. Here's the snaps and the malleable. Now we're gonna close the fascia. Kocher, please. The Rich back, please. I've got it. Just use the rest of the local in the small incisions and the most in the large incision there.
CHAPTER 16
So we've completed the case. That was challenging due to the extra padding or extra fat that was around the kidney, which sometimes we do see. This was a young gentleman who is tall and often they have some additional sticky fat to the kidney. I don't know definitively the reasons why, but I tend to see this in people that have taken some hits to the flank, either through martial arts or maybe they've played football or rugby. And so sometimes the fat is just extra adherent to the kidney. It's very important to try not to take the fat off in a way that also takes the capsule of the kidney off 'cause that is a challenge when it's reperfused into the recipient. And so there's certainly a balance between taking too much fat and then also not getting into the capsule, which I think was part of the component today. As far as indications, you know the greatest thing about living kidney donation is that almost anyone can donate. We take anyone from 18 to 75 at our institution and obviously they have a pretty comprehensive pre-op workup. First of all to make sure that they're safe for surgery, but then also to check the anatomy. And so in this particular case there was one artery and one vein, but sometimes we see people with multiple vessels or multiple ureters. So each case is thoroughly reviewed beforehand. And we use image guidance through a CTA to have a better idea of the anatomy that we expect in the donor. No longer do you have to be a perfect match to donate your kidney since we can do an exchange program. And so oftentimes we're taking a kidney out and putting it on a plane and then later in the day receiving a kidney for our recipient from somewhere else through an exchange program, which is a great advancement and allows people to donate when they're not perfect matches to their recipient. Addition of robotic-assisted technology for donation is something that several centers have been doing around the country for some time, but it's certainly not found at every transplant institution. I do think it is additionally beneficial, especially in someone like this patient who's very tall when we're trying to mobilize the kidney that's high, behind the spleen. I think it has added benefit in patients that are a little bit more obese, which is certainly something that we're seeing more and more of in our kidney donors with obvious careful selection of the donor to make sure that they're safe in the long run. So I do think this robotic-assisted technology has been a great advancement. Our living donors have a wonderful recovery. I would say the majority spend two nights in the hospital, but there are several that decide to go home on postoperative day one. So there's a chance this patient could even go home tomorrow afternoon, which has been fantastic. They do get a little bit of narcotic pain medicine if they require it in the hospital, but a vast majority of our patients actually go home and use just Tylenol, over the counter, for their recovery. And the majority of them at their one week follow-up are feeling quite great. And certainly at six months when I do my follow-up visit with them, many of them say that on a day-to-day basis, they forget that they've even donated a kidney. So, I think that while it is a major operation, as you could see, overall the donors do very well and have a long, healthy life ahead of them and a fairly quick postoperative course. So patients getting ready for a donor nephrectomy can do just about as any other preparation for surgery, which is to be as healthy as possible. And thankfully for most of our living donors, that is easy for them to do because otherwise they would likely not be a candidate to be a donor. But many of them are very active, which is a great way to prehab or get ready for surgery is to stay in shape and to be healthy. And certainly after donation it's really important that they maintain a healthy weight and live a healthy lifestyle to prevent having things like obesity, which can lead to high blood pressure and diabetes and can certainly go on to damage the kidney. So, all in all, healthy living before and after with a good healthy dose of exercise is the best thing for kidney donors.