Anterior Component Separation for Multiple Incisional Hernias Along an Upper Midline Incision
Transcription
CHAPTER 1
My name is David Berger. I'm a surgeon at Massachusetts General Hospital, and today I'm going to perform an anterior component separation for a mildly obese woman who has multiple incisional hernias along an upper midline incision.
CHAPTER 2
Let's open from here to here to start, okay? All right, go ahead. Making an incision. Use the knife, use the knife. Fat part of the blade, please. Fat part of the blade. That's the sac right there, right? Right. Fat part of the blade, just run it over. Don't make moves like that, just one move, smooth. Okay.
CHAPTER 3
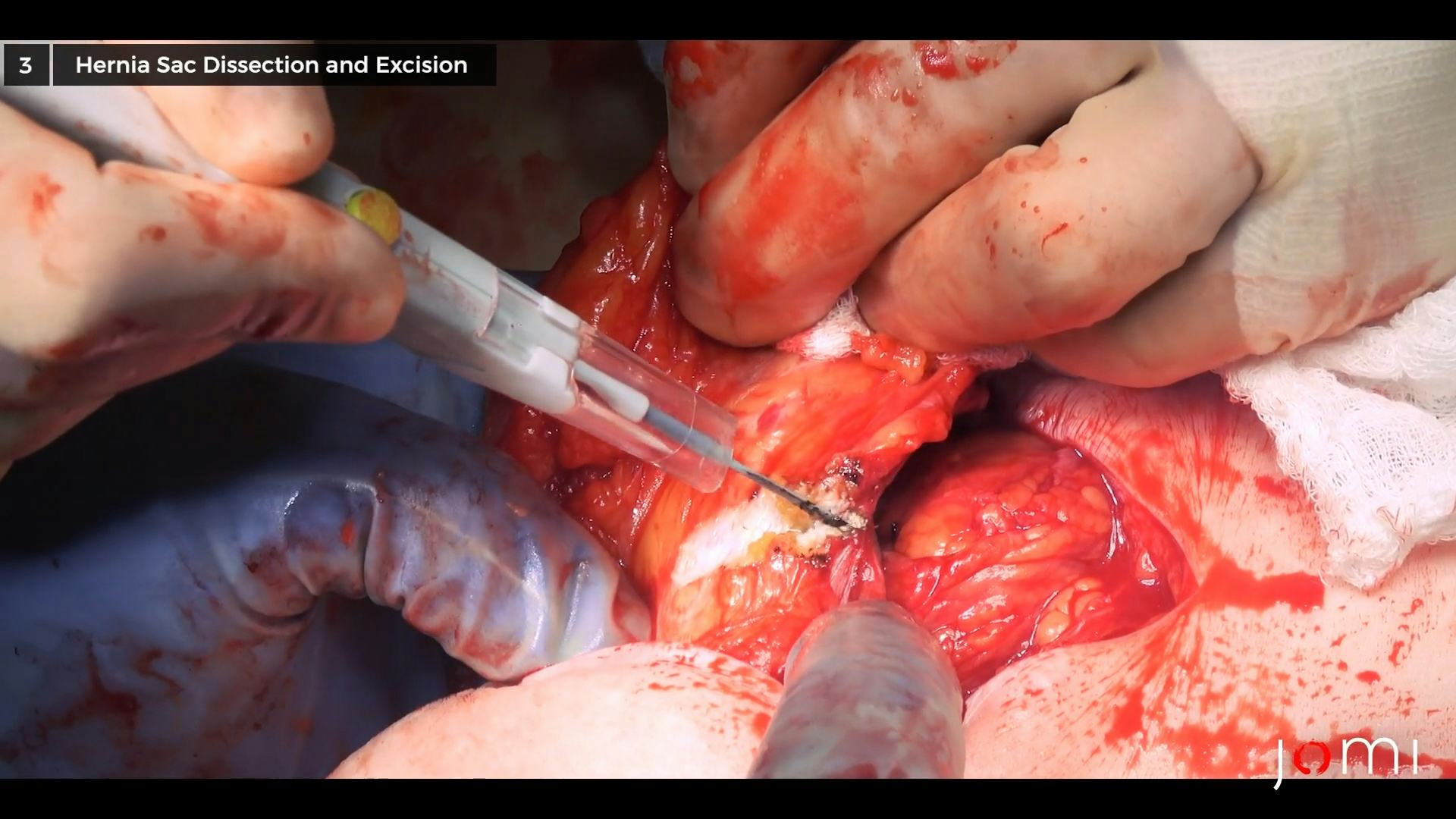
All right now pull. Get over the top. Get over the top, there's your hernia sac. Get your sponge in your hand, put your knife down. Okay, pull. Good, now grab the sac up, grab it with your sponge, and pull towards you, and we're just pulling the sac up off of the fascia, right? There's the sac, pull it up. Good. All right, now we'll go the other way. You may need actually a scissor or something to get that off, but we'll see. Okay. Hold on, you gotta let me hold it first. Okay, go ahead. Good, that's good. Okay, I'm gonna move down here, get more, go ahead now, pull. Pull. Very good, so pull that off there, yep, good, now I'm gonna grab down further. Good. Pull. Okay. There you go. See the fascial edges right there? Yeah. Good, that's great. Okay, now get your cautery. Hold on, I'll get this light right on. Get that light right on there. Pickups. Thank you. Just buzz that, yep. Okay, now go right on that edge, see it? Oh, look, here's the fascia. Lines, don't jab, lines. Oh, make another line there, yep, good. It goes actually this way. Now we're under here. Okay. Now, we have here... I think we may need to pull here, one sec. Yep, good. Okay now, it's right here. Yep. And then it's right there. It goes this way. Yep. All right, now let's just take that off of the sac, the underside of the sac. Great. Good. Yep. Oh, that's bad. That's bowel. No, no, up here. We need to fix that. Yep. Yep. And up here. Up here. No, no, it's right here. Yep and then right here. Yep. Yep. Yep. Yep. Okay, now there's the hernia sac, that's the fascial edge there. Yep. And then it's right there, see it? Okay, that's the hernia sac. Ah, no. All right, now…
May I have a pickup, please? Or DeBakey. Close. All right, we need 3-0 Silk, please. We're gonna need two 3-0 Vicryls. Stitch here to here. Do you want undyed or you don't care? Oh, I don't care. No, just a stitch right across the bottom. Yep. Snap, please. Another stitch, please. There. Yep. Snap. Vicryl, please. So you're gonna go inside out here to here. Did you get the serosa? I did, yep. Yep. And then you're gonna come back that way. Nope, no, no, no, no, no, here. No, here to here. Here, no, here to here. Yep. Roll there a little. You have to close it transversely, right? Yeah. Okay, cut. Now you wanna get up under the edges, right here. Yep. Now here. So that's... Yeah, this is the serosa, right? Maybe the serosa. Do you have pickups with teeth, or no do they not exist? No promises, they're... The rat tooth. That's all right, I'll take them. Good. No. Oh, no. No, no, okay. No, it's no good, Travis. Take that out. The serosa is this, right here. And the mucosa is there. Yep, that's it. No, you gotta get the mucosa. Yep, okay, stitch. Leave that on that side. Okay. Thank you. So don't - you have that stitch slid down. Okay, can I have a needle driver? Thank you. Tie this. Cut. Hold that. It goes behind. Okay, hold this this way. Can we get another Silk, please? There. Put a snap on it. Could I get a different snap from that one? Hold that for a sec. This should be dunking. No, no, no... Okay, let go. All right, tie these two over the top. You're lifting too much, Travis. 3-0 silk pops next. Cut. No. Righty or lefty, you're sewing? Pops? Parallel. Perpendicular, Travis. Yeah, but you've gotta turn your wrist to make it perpendicular. Yep. No, here, look for your last stitch is, you gotta move down here. One more. It's gonna be the last one. Yep, that's perfect. Yep. Okay. Hold on one sec. Yep. All right, cut. Get rid of those. Those are a little dirty.
Here's this. This is free all the way around. Almost. We gotta get this here, so we're not free there. Kochers, please. Another. Okay, give him a cautery, please. No, you gotta spread them. Okay, take that right there. Lower. No, no, here. You only wanna be on the white, remember? Yeah, just straight up fascia? Can I have pickups, please? Here, I can do with this. It's closer to me by a little. To me by - if you're getting the white, it's no good. There you go. No, that's falciform. Okay, see? Yeah. Now this feels like hernia here too, under here, so... And there's a hernia here as well. And a hernia here. So we're gonna have to open this up, and then we'll go down around there.
Keep coming? Yep. Okay, now you can use your cautery. Open this up here. Get in there and pull. That's a hernia sac, right there. Good pull. Good. Yep. So get right on this. Okay. Pull that back towards you. Grab the sac. Yep. Okay. Hold on. Sac right there. Right at the top back there. Good pull. Good, nice. Okay. Take it this way. Yep, go ahead. Okay, got it. Good, okay. So there's the next sac, right there. Yeah. So let's open this straight through. Lost a pickup, there. Okay, now see where the sac is? So go right to there. All right, and then it comes here, towards me. Okay. Now... Take that and hold it towards you. And then come right through here, right? This is a hernia here. Buzz through that. See, that's a hernia sac right there, right? Yeah. Grab that too. Okay, so here's our fascia, right there. Yeah. Yep. Okay. Okay, and then there's another hernia and the hernia sac, right there. Straight across. No, no, here. No, down to here. There you go. Then you're gonna pull that towards you. See the fascial edge, right there? Yeah. Yep. This way. Great. And some more hernia sac. All right, got that there. Now there's another hernia out here. So, open this up through here. Okay. Is this trash? Trash. Okay, and now the hernia is up here. So, come right out through this, up here. All right, but you want just a little farther, but - grab underneath there and pull towards you. Okay, good. And here's the hernia. So open this right here. This is fascia. Great. And then this is a hernia here, right? Right. Good. Great, okay, so let's take this off here. Yep, and then it comes right up. Yep, and right across there. Great, okay, so now let's feel on the inside of the abdominal wall. A little adhesion there. All right, feel if everything's free. Another adhesion there. All right, cautery. It's all freed.
Okay, all right, just bring out the omentum now, get this set so that we're good here, make sure there's no bleeding on this. Can we get the light on the field, guys? Can I have a pickup, please? Yeah, go ahead. All right. Buzz through that. Pickups and a Schnidt. Can I have a silk tie, 2-0? Okay. Another 2-0 tie. Good. It could be the side wall, but I just wanna make sure it's not this. All right, now let's start working on our flaps. Kochers, please.
CHAPTER 4
I only have two, do you think you're gonna need more than that? Nope, two's fine. So we're gonna have to take all this off. I don't know how much of this is gonna be viable, but - start right there, okay? Okay. Pickups to me. Cautery to him. Angle down. Lines. Don't dab. Nice, smooth lines. Pick it up underneath and lift, down here. Down to the fascia. Okay, hold on, over here. All right, you shouldn't be - you wanna just take your fingers and spread them up underneath. Okay, hold this for me. Come out here. Through here. Is that another hernia? That's what I was wondering. Looks like it. Yeah, that's a hernia right there. All right, so it looks like before we get to good fascia, this has all gotta go, here. So, go across here. And then right back up here. Down to that V. Right here. Yep, that's hernia sac there. Okay. More hernia sac. And you wanna instead of lifting up like that, you wanna lift under, up and under, that's the key. Yeah, you gotta get a little leverage. Yeah. Okay, hold that gently out that way. See - you're throwing your thumb back. I want you to do this without throwing your thumb back. So you're actually looking up underneath, okay? Okay. Too much, your fingers are in your way, you can't see. There you go. Okay, throw your fingers... There you go, closer to the fascia here. Okay. And here. And over here. Down here. Now we're moving out here. Can I have a step whenever you have a second? Okay, so that - yeah, and then you're slightly above it. Use your angles here, hold on. Think about what you're doing, let's see. I wanna get to the fascia. It's skinny there. All right, and a perforator there. Yep. Schnidts. Yep. Metz. Okay, tie. Just with your hand, reach over and hold that that way, gently. Okay. Yep. Okay, right up underneath there, Travis. I just want your fingers up underneath and lifting more up than back, right? Right. Here. Okay, there's a perforator there. Yeah. That one is small. You can take that, low - yeah, buzz me. Go lower on the fascia. That one's small too. Okay. Lower to the fascia. Your angle needs to be lower to the fascia. There's a perforator there. Buzz. Okay, buzz. Go through there. There's a big one there, right? Yeah. Schnidt. Another one. No, it's backwards. Yep. Yep. I need Metz. Okay, get up underneath there. Hold this this way for a sec. Okay, let's start up here. Here. Here. No, that's just scar, that just goes this way. No, no, no. It's here. Lower. No, lower. Okay, come here. Up here. Okay, right through here. Buzz. Yep. Okay. Lower. Good. Okay, what do we have going over here? Now this up here. Buzz me here. Okay, hold that up there. Okay, I like that. It's under here. Under me. A big perforator back there. Buzz me. Okay. That's good. Now we gotta get this upper part here, okay? So buzz right through here. And then buzz me, then buzz through here. Lower. Get your sponge under there. That light. Up here. Big perforator right there, see it? Okay, come up through here. That's hernia sac there, right? See that? Yeah. Yeah. Okay, so take that sac off right there. And then that right there. Okay, that's trash. Okay. All right, let's go the other way for a sec. Go ahead, you can go. Right here. The perforator right there. Here. Here's the plane. Okay, you can go through there. Pull out, not down. I mean, not up, pull out, not up, yeah. Move this over to here. Move that to there. Here. Okay, here. Yes, back here. Perforator. Buzz. Go ahead, buzz me, big perforator. Take this here. Schnidt. Schnidt. Yep. Okay, now we gotta move this way. Move this to here. You gotta go through here. Lower. We're gonna be here and here, right? Yeah. Lower. Lower. Perforator right there. Schnidts. Metz. Yep. Cut. Cut. Schnidt. Yep. Okay. Schnidt. Tie. Okay, let's keep going. Perforator there. Yep. Down to the fascia, yep. Can I have schnidts again? Yep. Yep. Almost there. Lower to the fascia, right? Perforator there. Yeah. Buzz this here. Can I have the light right here? I know it's here. Slightly lower to the fascia. That's a perforator, there. Schnidts, please. Good. All right, I think we have some pretty good flaps. This is good to here. That's good to there. This is not good. We need to cut this little bit off right here. So, take this. Yep, come right through here. Can I have a pickup, please? And then you can come this way through this scar right here, yep. Okay. And then, there's a hernia right there. Right through there. Right to the lower edge. See it right there? And then it comes across to here, yeah. So now we have fascia, fascia, fascia. Fascia on this side. And fascia here. This is just a little bit of falc - residual, preperitoneal fat, which we can take off here just to see better. It's residual ligament - falciform ligament. More trash. All right, so there's our defect. And it's a legitimate one. All right, so let's just cover this up like that. And let's do our releases and sew it closed. So…
CHAPTER 5
All right, we'll start on your side with the release. Okay. Kochers, please. Another kochers, please. I'm sorry. This light - this is nowhere near where we wanna be. Is that off? Yeah, can I have a lap? You gotta be up underneath. Big perforator, right there. Right here. Yep, Schnidt. I just took that one out too. Another Schnidt. Yes. Metz. Cut. Get up underneath for me, please. Okay, pickups, cautery to him. Okay, I have something from up here. Schnidt. How many? Just one. And a tie. Yep. Good. See it again? Okay. This one. Okay, so - there's where the muscle turns, so we want - let's lift this up here. We wanna release right... Right up here? Yeah, right there. We wanna release right here. And there's the release. And then we wanna come right here. And then it curves up here. Good. Good. That's it. Okay, now we'll release the other side. And the release line is going to be - take this right here. Perforator. Buzz me. Buzz up here. Buzz through there. Okay, so you're gonna start right here. Nice release right there. And then this is gonna go this way. And that way. And that way. Stay above the perforator. And that way. Great. And there's our release there. Let's just get that. All right, release one, release two. Go through to right there? Yep. All right.
CHAPTER 6
Number 1 Prolene, please. Get that light on there, yep. So she had what? About seven different hernias? Yeah. Make a move, yep. You need to grab the fascia. There you go, better. Pickups for one sec. Yep, got it, yep. One more. Okay, Schnidts to me, please. All right. Close this up. Actually, cut this needle here. Cut this one out here. I have two needles. Thank you.
Okay, let's just check for bleeding. Can I have a DeBakey. If you have one. Something right there. Schnidt. Pick that up. You don't have it. It's this stuff back here. No, behind it. Close, but... Yep. Can I have a tie, please? Cut. Okay. There's tiny, right there. Yeah, you can tap that. Okay, let's go on this side. Can I have the DeBakey back, please? Are you gonna need a couple more number 1 Prolenes? No, we're done. So pretty good release there, right? Yeah, absolutely. And this side, similar. Okay. All right, let's just see what our skin looks like here. Pretty decent actually. All right, drain, drain.
Out wider, out wider, yep. Okay. Knife back. Yep. All right. Hold on. Okay. Bring that up over the top. Cut both of these. Okay, nylons and staples. Local.
Make sure you put like at least 20 in the fascia, and then get the skin. Yeah, we gotta save enough for the skin too, although... All right, so we did a bilateral myofascial anterior component separation for a repair of a recurrent, recurrent incisional hernia. We have no specimens. It's a clean case. We put in two drains: one in the left flank and one in the right flank. And they look like, what, were they 19 Blakes? Yes. Yeah, 19 Blakes. So bilateral myofascial anterior... Component separation. Component. Separation. Yep. For a repair of a recurrent, recurrent incisional hernia. Okay. All right? Yep. So basically, what we're doing is we're doing a plastics flap by using the - there's three muscles on the abdominal wall out on the outside, three layers deep. So we open the whole thing up, take the skin off the muscles, and then we cut the external oblique at the top, out lateral. And what that does is that allows the middle part of the external oblique to slide to the middle. It's like the sliding glass doors, you know how when you have a sliding glass door, it fits in on the other door? Well, if you can imagine having three sliding glass doors, but it doesn't move, but you cut the lateral aspects so that you can then slide one of the glass doors across. Does that make sense? Yeah, I've only seen one done with mesh. For component separations, that's the whole idea, is that you don't have to do mesh. Oh, okay. I mean, I guess if you had a defect that was so big, that you couldn't do it without mesh, but the whole idea is to do it without mesh. For me, like I never wanna put mesh in somebody's abdominal wall because it's just the beginning of a problem, like a fistula, or an infection, or... So... You can take out mesh and put this in, right? Maybe that's what it was. Like that's what I would do there. Yeah.
CHAPTER 7
So, in performing the operation, I began by making a midline incision down over her previous incision and I encountered four large incisional hernias. We dissected the sac off of the fascia using a pulling approach, which elevates the sac up off the fascia and allows me to identify the fascial edges. Once I had done that, I cut the sac off and began to take care of the adhesions that were present in the abdomen. During that process, I made a colotomy and I had to repair that. We did that transversely with two layers. The first layer is running Vicryl, and the outer layer was done with interrupted 3-0 silk. We then completed the adhesiolysis in the abdomen, and once we had completely dissected free all of the hernias, we proceeded to raise flaps between the subcutaneous tissue and the anterior fascia. We did this bilaterally, tying off large perforators with 2-0 or 3-0 silk ties. Once we had gotten out towards the anterior axillary line, we then completed our myotomy or fasciotomy and incised through the external oblique fascia, allowing the fascia to slide to the midline. We did that bilaterally, and then I closed with a running number 1 Prolene suture. We placed 2-0 nylon vertical mattress sutures in the skin to evert the skin, and then we placed staples between them after we had placed two drains underlying each flap.