Trauma Resuscitation Demonstration in a Stable Patient with a Minor Perforating Wound
Main Text
Table of Contents
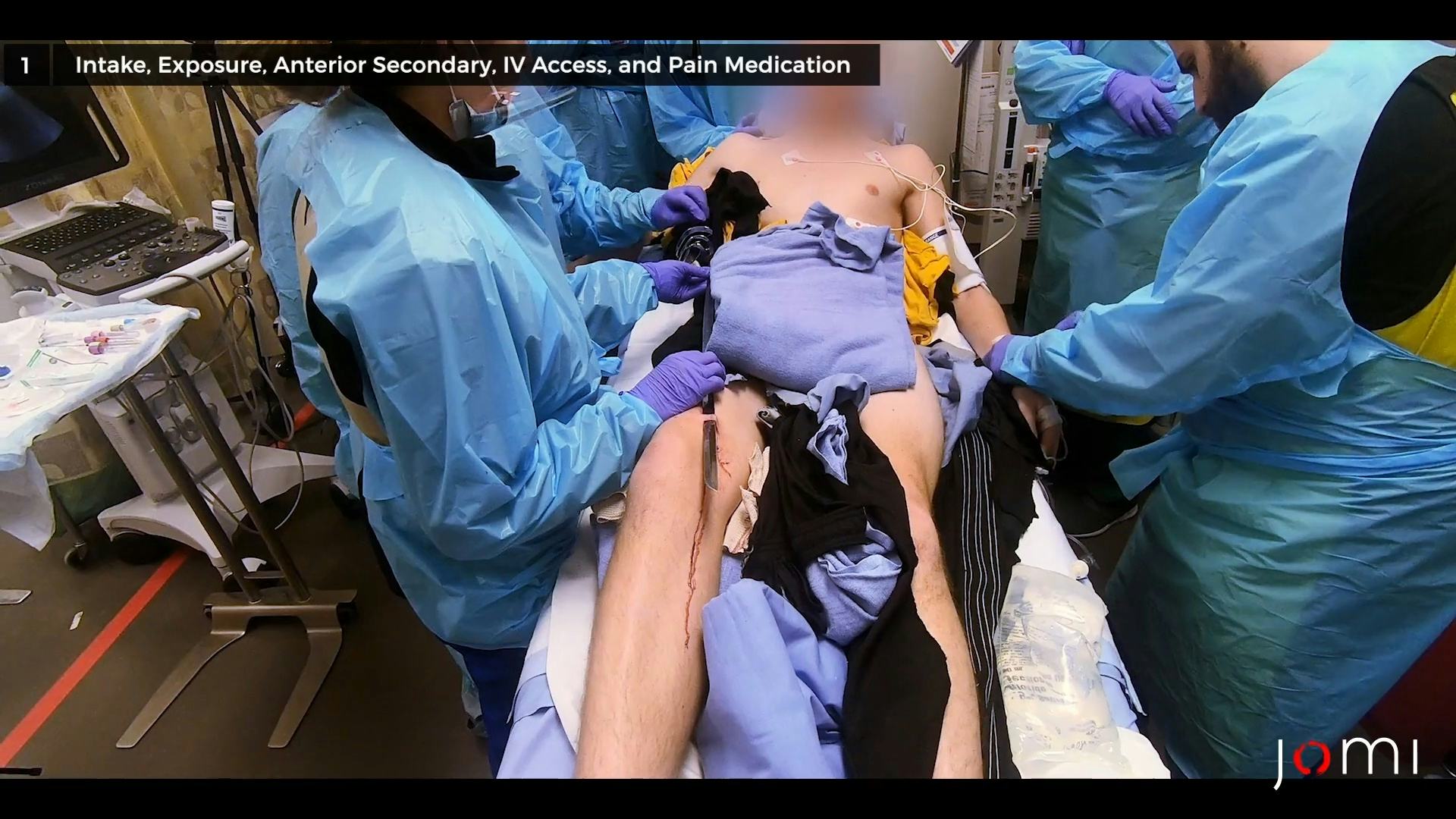
This is the case study of a 17-year-old male Reserve Officers’ Training Corps (ROTC) cadet who suffered a superficial perforating saber wound to the medial part of the right knee during a routine practice session. This video demonstrates the step-by-step patient assessment process and subsequent saber removal, providing a detailed account of the challenges faced by the personnel.
The assessment focused on understanding the circumstances surrounding the injury, taking into account the patient's health status and the specific anatomical details of the wound. Upon arrival, the patient was still holding the saber in place to stabilize it. The patient was carefully repositioned for further evaluation. The patient's airway was checked, and blood pressure was measured manually. The patient was laid bare for a thorough examination, and monitors were strategically placed to closely monitor vital signs. Vital signs and medical history including details about the tetanus vaccine and allergies were recorded parallel to physical examination. Intravenous (IV) access was established and fentanyl was administered.1
With the patient stabilized, the team initiated the delicate process of removing the saber. Precision is of critical importance to avoid the potential exacerbations of the injury. Following successful saber removal, the two 1-cm lacerations in the area of the right medial thigh were evaluated to ensure the absence of any signs of vascular injury. Preparations were made for a posterior examination to assess for potential injuries on the back, axillary, perineal areas, and the spine. The patient's movement was carefully coordinated to minimize discomfort. Additional injuries were ruled out. Before motor and sensory assessments of all extremities, the bilateral femoral and posterior tibial (PT) pulses were meticulously evaluated, ensuring the absence of any alarming indicators such as those of ischemia. The potential for an expanding hematoma or pulsatile bleeding were likewise excluded during the exam. X-rays of the right femur and knee were performed to identify potential fractures.
After completing the secondary examination, which included motor and sensory assessments,2 the arterial pressure index (API) was obtained. In the context of this case, the API played a pivotal role in assessing the vascular integrity of the affected limb and ruling out any potential injuries to the distal superficial femoral artery (SFA) and the proximal popliteal artery (PA). The API is a non-invasive and reliable tool used to evaluate the perfusion of the lower extremities. A blood pressure cuff was applied to the patient's injured ankle, and after it was then placed around the ankle of the uninjured leg in order to check both sides. The systolic blood pressure was measured at both ankles. The API calculation involved dividing the systolic pressure of the injured ankle by the systolic pressure of the uninjured ankle. A value of 0.9 or higher (generally considered normal) in this case, indicated adequate blood flow to the extremities.3 In cases of trauma, especially with penetrating injuries, a lower API might suggest arterial compromise and prompt further investigation.
Systematic assessment, precise execution of medical procedures, and effective collaboration between medical personnel are crucial in such clinical scenarios.4 This case serves as a valuable resource for healthcare professionals, offering insights into the critical aspects of patient evaluation and wound management in unique trauma situations.
The patient referred to in this video article has given their informed consent to be filmed and is aware that information and images will be published online.
Citations
- Fabbri A, Voza A, Riccardi A, Serra S, Iaco F De. The pain management of trauma patients in the emergency department. J Clin Med. 2023;12(9). doi:10.3390/jcm12093289.
- Clark A, Das JM, Mesfin FB. Trauma neurological exam. StatPearls. Published online 2021.
- Tung L, Seamon MJ, Dauer E, et al. Using arterial pressure index to predict arterial injuries in penetrating trauma to the upper extremities. Am Surg. 2023;89(1). doi:10.1177/00031348211011142.
- Khademian Z, Sharif F, Tabei SZ, Bolandparvaz S, Abbaszadeh A, Abbasi HR. Teamwork improvement in emergency trauma departments. Iran J Nurs Midwifery Res. 2013;18(4).
Cite this article
Prakash P. Trauma resuscitation demonstration in a stable patient with a minor perforating wound. J Med Insight. 2024;2024(299.4). doi:10.24296/jomi/299.4.