Open Cholecystectomy for Gallstone Disease
Transcription
CHAPTER 1
So we were presented with a 53-year-old male, who was complaining of right upper quadrant pains, beginning since last year. Now the pain was recurrent, and was radiating to the back. From his history, it seems that the problem involving- is involving your hepatobiliary area, so we... Workup was done, specifically an ultrasound, which revealed intraluminal gallstones. The liver was normal, intrahepatic ducts were not dilated, the gallbladder was particularly not thickened. So we had a case of acute cholecystitis, and when we received the patient, the patient was in a remission state. The recommended procedure for this patient, treatment, is to have your gallbladder removed. It's the organ that made the gallstones, and if we only take out the gallstones, the gallbladder will continue producing gallstones. So removal of the gallbladder is the standard operative procedure of choice. Now the standard procedure nowadays involves open cholecystectomies where you cut the abdomen from the right upper quadrant, and we have another procedure, which we call laparoscopic. The approach is different since we have smaller incisions- you can have 2, 3, or 4 small incisions, but the procedure remains the same, you still take out the entire gallbladder. In the urban setting, most patients are exposed to these offers, but in the rural setting, some centers do not have these equipment- the laparoscopic machines. And also, it's quite costly. So, people living in the rural areas could really not afford to have these more expensive procedures done. At any rate, like I mentioned earlier, the procedure is still the same, you end up with a removed gallbladder.
CHAPTER 2
All right. Cutting. Welcome everyone. For today, we'll be discussing a case of open cholecystectomy. So, I am Dr. Jun Soledad, surgeon is Dr. Enrico Jayma, and with us, is our first assist- sorry, second assist, Dr. Ted Carpio.
CHAPTER 3
We are presented with a 53-year-old male, with a 1-year history of recurrent right upper quadrant pains. On workup- abdominal ultrasound was done, which revealed presence of intraluminal stones in his gallbladder. There were no evidence of thickened walls and dilated ducts, intrahepatic and otherwise. Since the pain has been recurrent, he's advised to undergo removal of the gallbladder. So we begin the procedure by cutting through the right upper quadrant, making an oblique incision. So from the skin, we pass through the subcutaneous fat layer. We are now at the level of your anterior rectus sheath. Beneath that is your rectus abdominis muscle. So we will be accessing the abdominal cavity through the right upper quadrant. We are presently dissecting and separating, or cutting away the part of your rectus abdominis muscle. Depending on the patient's habitus and lifestyle, the rectus abdominis muscle can be thick or thin. Since we have a male patient, we expect this to be somewhat muscular, as you can very well see. Beneath this muscle is your posterior rectus sheath and then your internal oblique muscle. Sorry. Now the trick is to open the abdomen from the medial-most end of the incision. That way you will be accessing your falciform ligament and preventing or avoiding possible injuries to the internal organs as you begin the penetration into the cavity. Mosquito. Here you see the cavity has already been opened, this is your falciform ligament, your internal oblique muscle. The incision is made around one to two fingerbreadths from the rib cage or subcostal margin. DeBakey. On initial inspection, you see the liver edge here, the sharp border of the liver, you have her gallbladder beneath it with the fundus looking out. And inferior to that would be parts of your omentum and the end colon. So, we'll be pushing the colon caudally, and we'll keep it away using a wide Deaver. Or you can also use a malleable for- in this case. We shall also be retracting the duodenum towards the medial aspect or towards the midline. Now here is your gallbladder, fat-laden gallbladder. The liver appears to be healthy with no nodulations. The surface is smooth.
CHAPTER 4
Narrow Deaver. With the use of a narrow Deaver, we retract your duodenum towards the medial aspect. Ted, could you hold? So, the goal is to initially- find your cystic artery and ligate it. The procedure is less bloody when you dissect the gallbladder from the liver. We are now dissecting the area of your cystic duct and common bile duct, about the Hartmann's pouch. The cystic artery is a branch off your right hepatic artery. The cystic artery is accessed about the area of your cystic duct. DeBakey. There you go. Pickup. Pickup. We have just clamped your cystic artery, and we're about to divide and ligate it. Metz, please. So, the cystic artery is the blood supply of your gallbladder. Release. Yep. Around three of four throws.
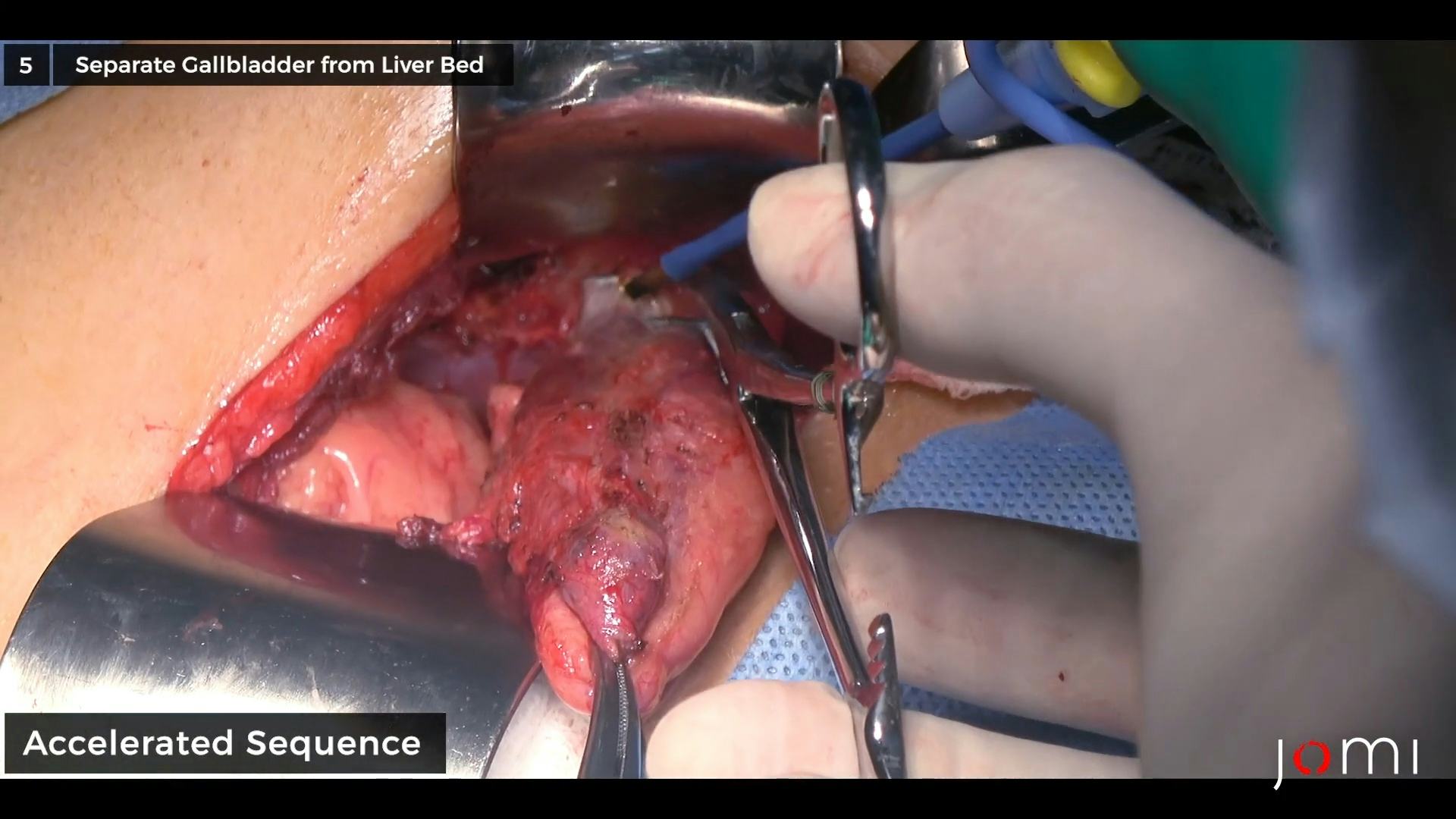
CHAPTER 5
Now once this is done, we can begin dissecting your gallbladder from the liver bed. So the trick also lies in the proper application of your retractors. This is your gallbladder fundus- as defined, it's the area of the gallbladder that is peeking out from the liver edge. It's approximate location is at the midclavicular line, on the right. Similar to all the other abdominal organs, your gallbladder is surrounded by a peritoneum, except at a certain area where it is directly intimately, or intimately related to the liver, and we call that the bare area. Now Dr. Jayma is now dissecting the peritoneal covering of your gallbladder. Cautery So, at this point, we're just taking down the gallbladder. Transferring from the medial to the lateral aspect, back and forth. Now this can be very difficult sometimes, especially if you have an acutely inflamed gallbladder. Now if the cystic artery has not been litigated initially, this procedure can be- sometimes be bloody. You might encounter a certain amount of hemorrhaging. Pinch, burn. There. Sometimes when the gallbladder is too distended, like in cases of hydrops, we sometimes drain what's inside. Initially. So the gallbladder is decompressed. So as you can see, we encounter less hemorrhaging, since we were able to initially ligate the cystic artery. This posterior side of the gallbladder is what we call the bare area, it's this part, which is intimately related to your liver, directly attached to it, occupying the gallbladder fossa of the liver. Now we are about to finish dissecting the gallbladder from the liver, just a few more peritoneal attachments. Mosquito. Now this is quite an easy procedure for Dr. Jayma, as he has done many open cholecystectomies before. We'll keep on dissecting until the gallbladder is left hanging by the cystic duct.
CHAPTER 6
Buzz. Ligate. Mixter. That is your cystic vein, and we shall be ligating it also. Metz. Tie. Release.
CHAPTER 7
So Dr. Jayma is now just peeling off- the adipose tissue surrounding the cystic duct and Hartmann's pouch. Good, good. Buzz. All right. Cautery. So this is now the fundus, the body. You have here your, your Hartmann's pouch, and beyond that would be your cystic duct. Your common bile duct is hidden away by this adipose tissue. So Dr. Jayma is now looking for an area where he can clamp the cystic duct and take out the gallbladder. There. Now once he's- once he's satisfied with his clamp, he can now remove the gallbladder. Good. Metz. Now that is your gallbladder. We shall be inspecting the organ after the patient has been closed. He's now applying ligature to the cystic duct. Before completely cutting the final ligature, Dr. Jayma will be inspecting the area of the cystic artery to make sure that the vessel is completely litigated. If there are doubts, he can apply a final ligature to that.
CHAPTER 8
Now before we close the patient, we do a final inspection of the operative site. Make sure there are no bleeders from the liver bed, from the gallbladder fossa and from the area of the cystic duct. So careful hemostasis is applied by electrocautery. Now, washing- is optional, we mostly perform that if we encounter spillages during dissections.
CHAPTER 9
After complete counting, we now close the patient layer by layer, starting from the peritoneum and the internal oblique muscle. Kelly. The first layer would involve your peritoneum, your internal oblique, and your posterior rectus sheath. Mayo. We anchor the suture at the medial end. You can also apply a wet sponge over the abdominal organs to avoid hitting them. Dr. Jayma is using absorbable suture. With continuous, interrupted method of suturing. We've just acknowledged that the OS count is complete. One more. We're almost done with the first layer of closure. Now the second layer to be closed is your rectus abdominis muscle. Now this layer involves the anterior rectus sheath and your rectus abdominis muscle. Again, the continuous interrupt- continuous interlocking technique of suturing is employed by Dr. Jayma. Dr. Jayma will now be approximating the subcutaneous layer in preparation for the subcuticular closure. Just a few interrupted stitches will suffice. Mayo. Now the skin is closed finally. using an absorbable suture, applying subcuticular technique. The wound is expected to dry up in around 24 hours, and heal by around 1 to 2 weeks. Now part of the advice that we instruct the patients is some recurring pains emanating from the operative site, specifically the scarred area. And this is usually felt when the patient shivers or- have, involuntary contractions of the muscle, most notably during cold temperatures. So we expect them to happen around November to February, and this is quite expected or normal.
CHAPTER 10
So, for this patient, when we opened him up, we noted that the ultrasound findings were fairly accurate, the liver was normal, the bowels were normal, the gallbladder was moderately dilated, it's physiologic. The walls were thickened, the intrahepatic ducts were also- not dilated, as well as the common bile duct. So after careful dissection, the gallbladder was eventually removed. The entire operative course was- quite uneventful, we did the procedure in under an hour. We did not encounter any bleedings during the procedure. Now postoperatively, the patient is expected to be fed immediately, and allowed to ambulate and to walk around. He is restricted from performing heavy activities for about 6 to 8 weeks, that is to take care of your incisional area and prevent incisional hernias from occurring. Follow up is usually recommended and suggested after a week, just to check on the wound. The patient can be sent home with antibiotics and painkillers. It is very important that painkillers be- given to these patients, because open cholecystectomies tend to be quite painful postoperatively, but it's not really that painful in, in the manner that you- it can be controlled by your painkillers. So, we have a lot of painkillers in the market. We can use any one of them, it can work for the patient. After about 6 to 8 weeks, the patient is now allowed to perform your heavy activities, he can even perform marathons, do weightlifting, get into active sports again. In the long run, the patients will, experience some bouts of pain about the area of your operative site. This could only be due to your involuntary muscle contractions during cold environments. Physiology-wise, there is really- no- discrepancy with the- between a patient without a gallbladder and a patient with an intact gallbladder. You see the gallbladder is just a storage organ for your bile, it's your liver that produces your bile, the bile's primary function is to digest fats in your diet. When we take in food, we take in carbohydrates, proteins, and fats. The pancreas and pancreatic juices in the bile usually takes care of your fat digestion, while your, your gastric juices and your small intestinal juices takes care of digesting your proteins and carbohydrates. So, if you take out the gallbladder, you only take out the storage organ, but the source of the bile still comes from- remains to be the liver. As I understand, based on statistics, as of today, gallbladder still runs ahead- from the- from appendicitis case, so, it's- we encounter more, gallbladder stone cases, even compared to appendicitis cases. So it's not really a rare condition, the procedure is not really rare, you know, a lot of surgeons rapidly perform more gallbladder surgeries compared to other procedures. Patients come in and ask us if- what could they do to prevent gallstones from occurring? It's actually a metabolic thing. If you are a stone-former, you will really form stones. It's in the way your gallbladder digests and metabolizes fat and cholesterol. If you are a stone-former, you can't really avoid- having stones formed. But the thing is, mere presence of stones, does not really- it's not really mandatory for a surgical removal of your gallbladder. It's when your gallbladder becomes diseased, that's when- that's the only time when surgeons recommend removal of your gallbladder. So it can be diseased if it becomes inflamed from obstruction. So it doesn't really- matter whether you have a few stones, or a lot of stones, or a solid-type of stone, it doesn't really matter whether you have small stones or big stones. What matters is if your gallbladder becomes diseased due to these stones. So, complications arise if your gallbladder- causes obstruction in your cystic duct, preventing bile from coming out of the gallbladder, or if small stones accidentally passes through the cystic duct into the common bile duct and causes obstruction in that area.