Partial Laryngectomy Techniques (Cadaver)
, Duke University Medical Center
Transcription
Today we're going to go over some conservation laryngeal surgeries: supraglottic laryngectomy, supracricoid laryngectomy, with cricohyodopexy, or - cricohyodoepiglottopexy, so that would be CHEP. And they address specific indications.
The first indication is, one, you've got to be sure they've got good pulmonary reserve. Some people say greater than 60 is a risk, but I really think it's more pulmonary in just their ability to functionally rehabilitate.
CHAPTER 1
The external supraglottic laryngectomy is - it was designed for tumors isolated to the supraglottic larynx that does not transgress the laryngeal ventricle and involve the glottic larynx. They can involve the pre-epiglottic space, they can't have extralaryngeal spread. The supraglottic laryngectomy - you can include the hyoid bone, and you can extend it to include some of the tongue base, but the risk of aspiration is worse once you do that.
The supracricoid laryngectomy was designed for supraglottic tumors that transgress the glottis or glottic tumors that extend up to a centimeter into the subglottis anteriorly and no more than 5 mm posteriorly because the joint is much higher, it's about 3 mm - the arch is about 3 mm below the posterior part of the cord posteriorly. You have to be able to save the cricoid. Literature says you can take one arytenoid. If the arytenoid is fixed from tumor and you pop it and the arytenoid joint doesn't move because tumor, that's a contraindication because you'd have to take the cricoid.
It's my opinion that you shouldn't have to take the arytenoid cartilage at all because most of what you see is mucosal involvement, so you can preserve the cartilage itself, and the joint, because if you were to have to take the cartilage for a margin, it's probably going to be in the joint. So, you have to read it carefully. It's best if you can just take the mucosa off in the vocal process and save the arytenoid, the patients will do much better.
The other point to remember is, why this potentially even works is, most of the - Hirano talked about most of the phonatory glottis being the membranous cord, and the airway as being from the vocal process posteriorly to the interarytenoid area. So that is where most of the breathing occurs, so you can take the cords and still have a decent airway because most of the laryngeal airway is between the arytenoid cartilages. So that's one little variation, I really don't like to take an arytenoid on either side. And it's contraindicated if the joint is actually invaded. And you only know that by palpating.
So, Adam's made a nice incision here, I'll just open it up and show the anatomy for the supraglottic laryngectomy, because if I do that, it'll mess up the rest of the dissection.
Once you've exposed this, what you want to do is - if you can, in a supraglottic, you want to save the hyoid if you can, and you can divide the straps at about the level of the thyroid cartilage, the upper border. You do that in a supracricoid laryngectomy also. If the tumor is up against the hyoepiglottic ligament, I think you should take the hyoid and a little bit of the tongue base as a margin in a supraglottic laryngectomy. In a supracricoid, you have to be able to save the hyoid, or - there's some recent reports where you can kind of extend it, but ideally you'd like to save it. You don't want the pre-epiglottic space up high significantly involved because you can't get a margin, so it's really for low and for hyoid tumors that transgress the glottis or glottic tumors that go infraglottically. The contraindications are, you can do it for a T4a, but if it's through the thyroid cartilage, you can't do it. If it's extralaryngeal, you can't do it. If it's more than a centimeter anteriorly, you can't do it. When it's in the interarytenoid area, you can't do it. The pulmonary function is a contraindication, and cricoarytenoid joint fixation is a contraindication. Otherwise, you can pretty much have at it.
CHAPTER 2
So what I'll do here is, I'll just first - let's just cut. Top of the thyroid is there. I'm just cutting the omohyoid and the thyrohyoid muscles here. And then - do you want to just elevate that, Russ? Let's just elevate and leave it on the - on the hyoid. You don't want to ever get up and cut the suprahyoid muscles, because if you do you'll devascularize the hyoid. So we'll leave it - there's the sterno at the thyrohyoid.
Okay. So - Let's divide this, too. The thyrohyoid. Just be careful not to get the superior laryngeal nerve, there. Just remember, the superior laryngeal nerve is deep to the - superior thyroid artery, enters the larynx - if there's the superior cornua and there's the notch there, it enters a centimeter anterior and a centimeter superior to the notch, so it's going to be entering the thyrohyoid membrane about there. So if you just stay on the thyroid, you won't injure that.
CHAPTER 3
So when you do a supraglottic - at this point you've got a trach in - the main thing is, where is the location of the anterior commissure. Okay, in a male, if you - here's the notch, and here's the bottom of the - of the, uh - the top of the cricothyroid membrane. In a male, if you go halfway between there and the notch, the anterior commissure inserts at about the midpoint or a millimeter above, so you want to make your cut above that, like that, for a supraglottic. In a woman, go up about two-thirds, it's a little bit higher. What you don't want to do is go too low. You can always take more, but if you take Broyles' ligament with it, you've kind of messed up the operation, so -
And the other trick is, if you can - in larger larynxes - this is a small one, but in larger larynxes, you can actually feel a depression. I can feel one about right there. And that's very prominent in a man, and that depression is usually where the anterior - the top of the anterior commissure tendon is. And you can just see, it's about right there, so - you'd make a cut like this.
And then - so once you do that, you can release your constrictors here, you can take your superior neurovascular cartilage on both sides, you can cut - either take the hyoid, if you take the hyoid, I'd suspend this to the mandible, but if you can save the hyoid, you basically cut the muscles here, the infrahyoid musculature. Stay underneath the bone, get into the vallecula, pull the epiglottis down, take the vallecular mucosa, and you make your cuts laterally and connect here.
Once you bring that forward, you can see where - I'll show you that later, but you'll see where the arytenoid cartilage is, you'll cut just in front of the arytenoid, and then you'll get into the posterior aspect of the ventricle and you put your scissors right into the apex of the ventricle to the anterior commissure on the side away from the tumor. Then you just flip it over and you make the cut the other way and you're basically done. And then you just resuspend it with a couple of Prolene sutures submucosally, hyoid to thyroid.
You can do a cricopharyngeal myotomy. I haven't done that a lot because I think reflux is significant and most people I've seen that get supraglottic tumors, a lot of them are really overweight and, you know, they're refluxing, so I tend not to do a myotomy in these patients, but that's very controversial.
So, are there any questions on the supracricoid laryngectomy?
CHAPTER 4
Okay, you're basically taking the whole pre-epiglottic space, which is the thyrohyoid membrane down to the petiole, the false cords, you're taking all the quadrangular membrane and the periglottic space up high, and then you're taking the hyoepiglottic ligament, the epiglottis, and leaving the hyoid. So you've encompassed all the fat in there.
What I've always been nervous about doing this endoscopically is that for higher tumors, the tumor will go through the perforations in the hyoid and then get in the epiglottis and then into the pre-epiglottic fat. I'm never comfortable with that margin, but this will actually encompass all of that, and I would actually prefer to do this in a radiation failure because you know you've got a good margin, where you really don't know if you're leaving pre-epiglottic fat in endoscopically.
Alright, so, the - supracricoid laryngectomy with cricohyodopexy is - basically designed for glottic tumors with subglottic extension or a little bit of supraglottic extension on the false cords, because you resect the false cords, the AE folds, but you preserve the epiglottis and by definition you're preserving the pre-epiglottic space. For supraglottic tumors that transgress the glottis in the anterior commissure, you have to do a supracricoid laryngectomy with cricohyodopexy, and you take the epiglottis because you've got to clear the pre-epiglottic space. So, they're different in this way.
If you do a supracricoid and you preserve the epiglottis, you are making your incision - right here. Do you want to buzz through that or cut through that, Russ?
So you're going to just stay on the top of the thyroid cartilage and then you're going to elevate. So if you just stay there - yep. And we do that on both sides. So you can elevate here. Just elevate the perichondrium off a little bit.
This is the way they're exposed to approach a laryngocele, too, externally. You can take down this ala and just take the laryngocele out that way. That's an external approach.
Okay, then what we want to do is free up - you can feel the epiglottis here, and this is where we're going to enter, right here, and then cut the epiglottis till we can see the aryepiglottic folds. The other thing we do early on is we're going to make a cut on the top of the - make a cut on the top of the cricoid. And we'll put an endotracheal tube in there.
Keep going, yep.
And this is where you want to look, make sure you're negative at the bottom of the cricothyroid membrane.
How far away do you want that margin to be, for you to feel comfortable?
Well, if the - it's supposedly contraindicated more than a centimeter, right? So if you're - if the - the apex of the ventricle is considered the top of the glottis, and the average width of a vocal cord in the midportion is about 5 mm, you're talking about 5 mm, plus you're going to have at least 5 mm of the thyrohyoid membrane free. There are reports of - when it's lower, people have taken the anterior part of the cricoid and doing basically a hyodotracheopexy. But I don't have any experience with that, I don't know how they do it. Has anyone - have you done that? But they have extended it down that way.
So now you've got your tube in there, you want to release your constrictors on each side and being careful not to injure your - see your superior laryngeal nerve right there? You want to get all the way to the joint because we want to disarticulate the joint.
Keep going here, I think. Got a ways to go.
You see that?
Mhm.
Okay. Are we there yet?
There's the arch. There we go.
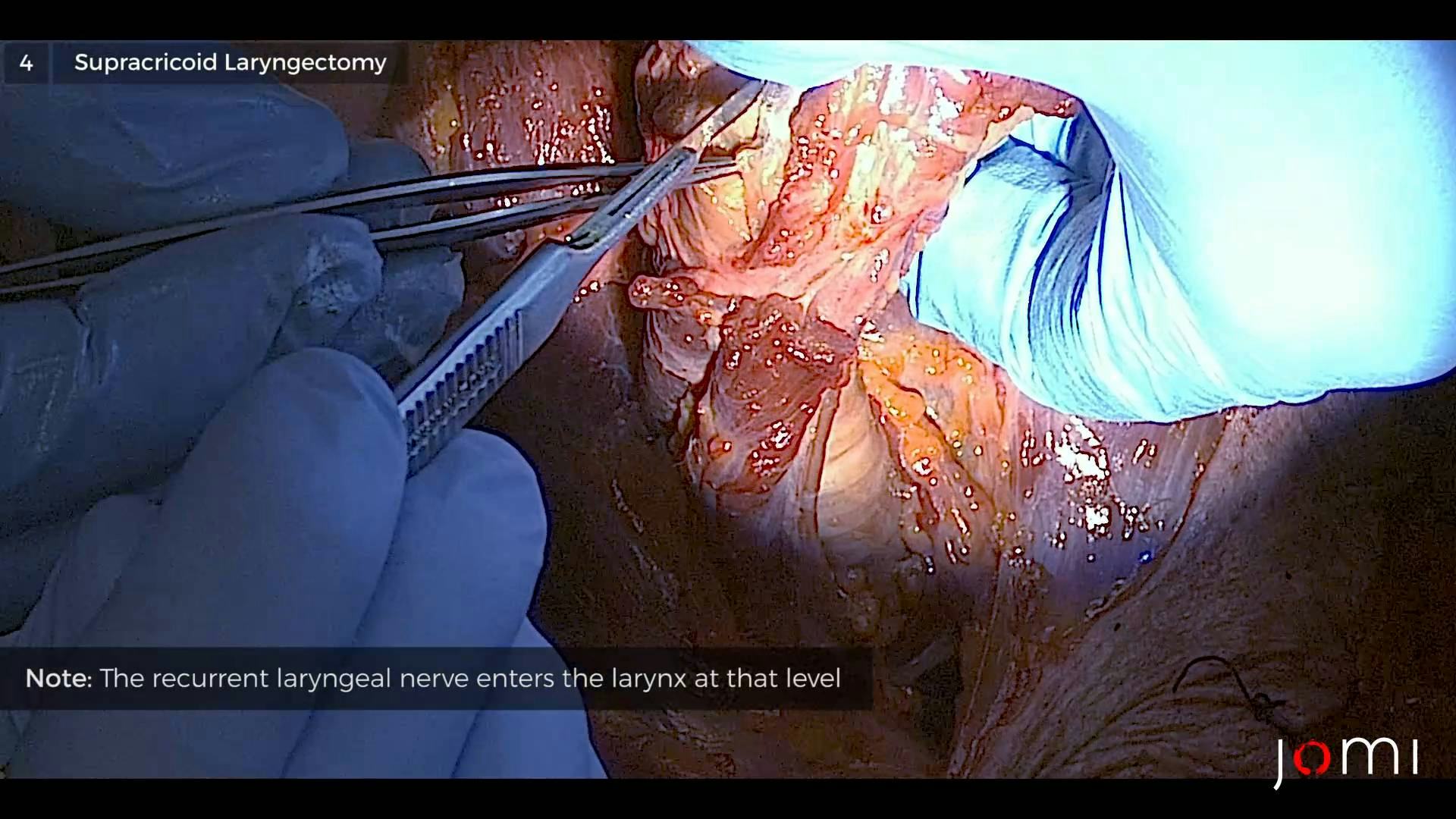
Okay, we have to be careful here and stay on the medial aspect of it because the nerve is going to come right underneath the joint. It's going to enter the larynx right here. So, here we want to stay kind of subparachondrial and release the joint there. There we go.
So - Once we have that - thank you - we release the joint. So that's the cricothyroid joint right there. So the nerve's going to be there. If we dissect it, we should see it. I think we're getting a hint of it right there. This is where Crumley's described finding the nerve and hooking it intralaryngeally when the nerve has been cut high in a thyroid for an ansa. You actually will divide the cricothyroid muscle, find the joint, take it down, and find the nerve in there. He says he's had success, I've never done that.
So we've got that free. And then we do the same thing to the other side. Can you get to that, Russ, at all? And then we'll free the joint up here, too. Not going to worry so much about the nerve, but that's what you do, basically.
So now we've got the laryngeal framework free. We'll now come up here and - try to preserve the hyoid.
So here is - there's a nice illustration of the hyoepiglottic ligament right there. And that's pre-epiglottic fat. So that is a barrier to tumor spread there, unless the tumor is huge. So we'll try to take this down on the undersurface.
Pull that. And you just pull it down here. So we'll take this all down.
There's epiglottis.
So you're seeing epiglottis right there.
Yep. That's all epiglottis here. And then we want to enter the vallecula up here. That's the median hyoepiglottic ligament there.
Okay, so - There we go, there's the vallecula. Just going to cut into it. You can see, get a hint of the epiglottis right there. We'll open that.
Is there a pair of Mayos around anywhere? Thanks.
So - Now we're looking at the epiglottis, here. So here's the epiglottis. So now we've basically encompassed the pre-epiglottic space.
Let's take this down.
If you look at the pyriform sinus here, hopefully you'll see some sensory nerves coming down. You want to try to preserve those because those'll go to the arytenoid. And once we get this, here's the pre-epiglottic fat. So we'll just make this cut to clear the pre-epiglottic fat right along the epiglottis.
Now this is the key move here. You see here - you'll see here, this is cuneiform cartilage here. This is corniculate cartilage. And this is, actually, the arytenoid cartilage. So often, when you're starting out, you look, and when you're scoping these people, you're seeing tumor on the corniculate or the cuneiform cartilage, and the first thing you think is, well, the arytenoid's involved, when it's actually not. So you've got to be sure it's actually on the arytenoid. The corniculate and cuneiform you can take inconsequentially, so - what we'll do is - thank you - it's right here, so if you can see - So I'm going to take a cut right down the posterior part of the AE fold because that is the quadrangular membrane attaching onto the arytenoid cartilage.
Where is the glottis, here? There it is.
So now, here, you can see this is the back of the apex of the ventricle right there. So I'm going to make this cut right to the back of the apex, this way. And then now, I'm going to take all of this. Okay, you can see - Almost there - There's the - the thyroid cartilage is here.
So here's the pyriform mucosa, and we're going to save as much of that as we can. Right down to the apex. Now you can see, there's the medial wall. That's cuneiform and corniculate cartilage here. As we're looking here, there's the apex of the ventricle, right there. Does everybody see that?
So this is the true cord. So now we're going to cut the true cord and the vocal process right down to the cricoid. So there's the top - where's the top of the cricoid, here? Now we should be able to make a cut across - We should be able to connect our cuts here.
There's the joint.
So now we've got it opened. So now we're going to make this cut right along the top of the cricoid, which we've done. Now we've got the larynx opened.
So you can see - there's the cartilage. We've cut the vocal process. Now, here's the other ventricular apex, right there. So this is the - this is - cuneiform cartilage, it's separate. This is corniculate here, and the arytenoid is actually this cartilage here. It's right there. So these 2 cartilages lay on top.
So what we want to do here, again - this is quadrangular membrane right there, so we want to cut right here to the back of the apex of the ventricle. Right there. Then we're going to cut the vocal process. That's the cord. Down to the cricoid. Just basically connect these dots. And then come right up the joint.
We separated this?
Yeah.
Not quite.
Again, so this is - that's the lateral wall of pyriform, right? Should've freed this up just a little bit better.
Okay, there we go.
And that is basically collapsed, so now we've just got this cut right here. Can you get that cut, Russ? I've got to hold it up. It's just this cut right there.
So we're just cutting across the back edge of the conus elasticus attachment on the cricoid.
So that's your tumor. So you can see you've got the whole epiglottis. You've got a nice illustration of the laryngeal ventricles. There's the petiole. These are your true cords, your periglottic space, and your pre-epiglottic space has been removed.
So, that's that. If we were to do a cricohyodopexy, we would've entered here and made the cut right here. And this would've been left up for a subglottic tumor.
CHAPTER 5
So how do you fix this?
Call Dr. Puscas?
Call Dr. Puscas. Here we have the hyoid. You want to release the larynx. Just develop your plane here in the anterior midline to pull the trachea up. You put - I like to use 2-0 Prolene permanent sutures, you put 3 sutures: one in the midline around the cricoid submucosally, and then - around the hyoid, the tongue base, and back. Then you put your next one 8-10 mm apart, like that.
Laccourreye, who talked about this, talked about - now you've got the posterior cricoarytenoid muscle pulling on the arytenoid and rocking it back, so what they say to do is to try to recreate a T - I don't understand this, but you want to take a stitch, like a Vicryl, through the vocal process and tack it to the, um - to the cricoid, so that you get this. You get a T there, so that when it opens - because the arytenoid rocks on a joint like this, so they want a little bit of opposition this way. So you can just sew a little stitch from there to there to hold it like that, because they want this looking like a T.
So then once you've done that and pulled this closed and you've tied your sutures, and you take your straps and sew that to cover it, that's all you do. You don't close anything else, you put a - you put a Penrose and a wrap, and then the last part they talk about is taking the pyriform sinus mucosa and resuspending it by taking - let's see - here it is. So you've got this pulled up and I'd like you to take this pyriform sinus mucosa here and then put a couple of stitches here and then reapproximate it to the other side to kind of bring the anterior wall forward, the anterior wall of the pyriform sinus forward and kind of recreate what that looks like. Then you lower your trach, put a neck wrap and a Penrose, and that's basically it.
Is that clear? As mud?
So um, for that arytenopexy, you don't try to - it's just a holding suture, you don't try to - connect the mucosa together?
No, no. We actually don't so it doesn't stenose. All you're trying to do is put a little - just a little forward tension, because you've cut the vocal process, and now it all just kind of folds back, right? So you just want to keep it just a little bit forward, like that, just a little - that's just a stitch, like that. And then this will get pulled up to the tongue base, like that. That's your closure, you put a couple of those stitches there to recreate your pyriform sinuses, and that's - you're done.