Whipple Procedure for Carcinoma of the Pancreas - Part 2
Transcription
CHAPTER 1
So let’s - where’s her pylorus? You don’t have to get it all in one shot either. Get in. Take less. Take less, yeah. Alright, so now that’s - that’s the pylorus. So there’s two ways of doing this. You can do a pyloric preserving or not. Some people even do like a take out the whole antrum too. I don't do that. You can also even potentially hook up the pancreas up in the stomach when you do your reconstruction. Occasionally, some people will do that. So now this side, so where’s our pylorus again? So I was fooled before - there.
Well this is all heart, unless this is pancreas sitting on top. It’s all just pancreas that’s lying on top. Yeah… Go through that. See the portal veins right underneath this? Just cut that.
So this is the pylorus. Yep. Okay, I might need to reload. Yeah. Go on your side just a little bit - yeah, yeah. So we are going to come… Well, let’s take some of it down before we divide it. So this - you got to find the Ligament of Treitz. Yeah, do you know where to find it? You could do that. Flip up the transverse colon, and it’s the only loop of bowel that’s going to be full parium - which is right here. So you - you want to take some of it first before we divide it? Debakey. Alright, let’s divide it.
CHAPTER 2
Turn it around so that it’s… Right on the bowel. This way we don’t run into anything important - take one more. One more should do it. Okay. Hold that. How’s she doing?
Thank you. So lift up her bowel. Okay. This is all the mesentery stuff - this stuff will bleed. You get too far away from this - you’ll run into the IMV. Connect your dots. Right through the perineum. Get your ligature on that stuff - or you can - or you can get that stuff on my side - on our side. That’s just the peritoneum. And right down here. Okay, good. Swipe - pancrease - get your ligature now - sit right on the bowel.
I would turn it the other way, right? You thinking, because it goes along with the - here let’s get this, little bit of that stuff. Careful not to tear up there, just over here, okay? Cuz let’s hope - hopefully will bleed there. Okay, good. Down here just a little more. Alright, good. Come back over here.
So this is the duodenum. We’re taking it from - we took it from the Ligament of Treitz, and we’re moving it from, you know, the Ligament of Treitz, going underneath the super mesenteric vessels, and getting it to the other side. That might bleed. A little bit of that. That’s good.
Get your ligature on this stuff. Yeah, that’s - that’s what I suggested, I think. Come closer to me if you can. Yeah, right there. Okay. Let’s check Bovie. You think? Just a little bit of this. Should be able to swing it all underneath now. Alright, see if you can get it through - you can probably get a little too much in this side but… Yeah, all the way to the other side. You got to feel from this side though. Come over. That’s okay. Alright. That’s pretty good. No - no - that’s fine. That’s easy. That malleable - actually, can I have a short right angle instead?
So this is the pancreas. It’s normally a different color, but her’s is pretty fatty. So we're going to divide this in a second, and then underneath this, see here’s the super mesenteric vein and here's the portal vein, so right underneath it, everything - so then we’re going to divide this, and then I’ll flay open, and then we’ll take the pancreas and uncinate process off and that’ll be our specimen.
CHAPTER 3
We divided the bile duct, we divided the stomach, we divided the small bowel - so all we have left is the pancreas. You can still turn back at this point in time - but once you’ve done this, you have to do everything - yeah. So take a big chunk like over here - all this. Yeah, a big bite. You can tie it - tie it down, because there’s a vessel in there too. Yeah, most of the - most of the time. Doing this, I don’t get the - careful, it’s going to tear - so you don’t want to be too hard. Yeah, so that one’s going to be a little more difficult. So that’s one’s going to be a little bit more difficult, right? Because you got all that stuff there. So you’re going to take all this stuff here, you know what I mean - you? Take all this and come out but you don’t want to get the vein underneath.
Alright. Bovie. No, just take it. When you get to the pan - the duct - just go. Nah. All this stuff bleeds like stink. You got to go straight the whole way. Get that - don’t just Bovie it. Please let it stink. Keep going. Don’t - leave that one alone because I don’t know where the duct is now.
This all has to go. Yeah. Hold on, let’s - there we go. It’s too thick to do - so if you do that, I would go - I would go - you’d have to go like - like this direction as opposed to down because this way is too thick. If you do it he other way, it’s not. Okay, yep. Sorry. I didn’t think there was an opening there. Yeah, it’s right there. Yeah, I see where the…
So this is the port SM - super mesenteric portal portal vein. This is cut in your pancreas. Yeah and this is splenic vein is right here. Right, yeah. This usually comes down - yeah, that’s pancreas. This stuff we have to slowly take. There’s always stuff in it - usually - okay. I usually do that but go ahead before I tear it. Stay close to you. So this usually - see this knot much? Every once in awhile, you get a little something, and the duodenum actually helps. So part of the problem with the stuff down here is - no, no this all retroperitoneal stuff. Go ahead - don’t go too deep. Try not to go too deep - it’s more superficial. Yep. Careful. You’re fine - just cut it. There’s - there’s nothing in there, right? SO you don’t have to… Okay.
I’m trying to get the retroperitoneal stuff out cuz that’s where you’re going you’re going to get all your lymph nodes. Just Bovie that. We’re just going to get these little branches in here. Nice big ol’ lymphatics. Let’s see where we’re at on this side. Alright, so we haven’t divided that quite yet - almost, but not quite. Might be something in this. No, just Bovie slowly. I think - whatever it is, it might be underneath it. There it is. Yeah, you can ligature. It’s going to be hard because it’s going to be flimsy, so try not to rip it. You just go straight down on it and stay off the vein, see the vein? Come off of it more. Come off of it more. You might have to Bovie it now. Come down where - I’m trying to figure out where the artery is. We got a little bit of work up top. Over here we’re almost done. So I would… So stay right off the vein. See the vein? Okay, okay, just want to make sure.
Okay, here’s the vein here. Just keep rolling along - that could be a branch here. It does roll, and - you have to try not to. See, here’s a branch or something here. Bovie that. Let’s see. So I’m staying away from this stuff in case it is a branch, I have a little bit of a - staying away from the vein, staying closer to the specimen side - so in case I get in trouble, I have a little something to grab onto. Let’s see if we can see something. See this stuff here? Take that - that’s not the vein, right? It’s going to go from there to there, but there’s where the vein is. So that your stuff here. Yeah. Okay, hold up. This is going to be a branch maybe. Metz. See if this were another vessel, I’d pull it over to the side - oh, you can. I - I wouldn’t grab little bites with it though - I’d take a big bite like any large vein. Bovie this. See where you’re going? Yeah. Good, good.
This side is going to bleed - my side. Alright. No. Yeah, there’s not enough room. You could tie it. This won’t work. I can tell you right now. Alright. Go ahead. Get your ligature on that. So I got this. Go ahead. Yep, take it right there. Yep, right there. Good, perfect, okay. Didn’t do anything to her. Okay. A little. Okay.
So I want to get all the way over to where the artery is, so we’re pretty close to it now. Okay. Get your ligature, come across this stuff, so we’re right on the artery here. Your finger is - this is artery right here. We’re already beyond it a little bit. Go like that - yep, right there - take it - yep - yep, take it. Come and take all the stuff right up to the artery, which is what we’re doing. Get your ligature. Cut the big one. No, no, lower. Yep, right there. Hold on - hold. Okay. Yeah, we go a little higher - yeah, above it. Yeah, I want to get that little thing - yeah, right there. Take it. Take out the artery that’s in my hand.
This is the artery. Yeah, this is the artery. Alright, so we want to stay - yep, right there. Take it. Alright, duodenum, bile duct, gallbladder, stomach, pancreas. Alright, keep this stitch Brian, and after I screw this all up here. Here it is. Put a stitch - see the little - that’s the pancreatic duct. Put a stitch there and tell them that - so can we get a pancreatic duct margin, that’d be great. So as you can see, that’s where - this is vein here. And this is the artery here with a big ol’ pulse in it here. So right on it and actually underneath it. Here’s the duct, nice and big. This is a stint they use for eyeballs. That’s pretty good. Yeah, that’s great actually.
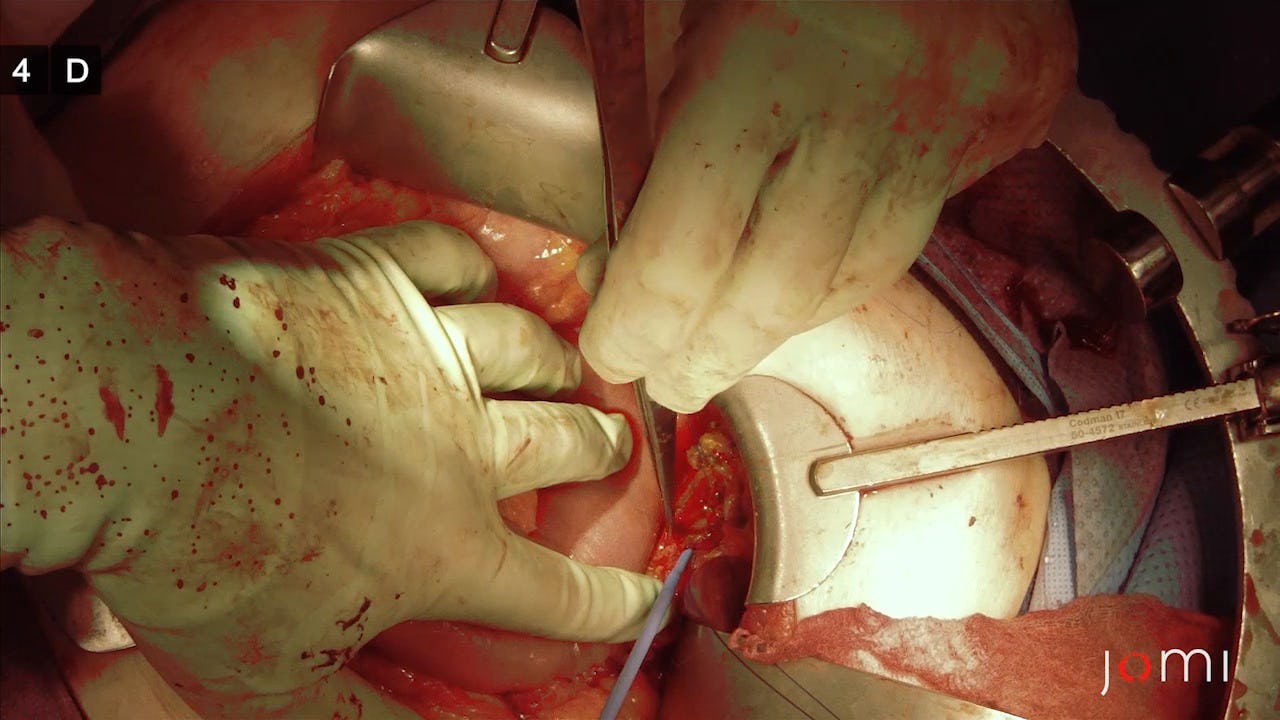
CHAPTER 4
Here’s the splenic vein right there, and here’s a little branch. So you’re going to go to pancreas to surosa - pancreas to yeah. So you’re going to do a couple of these in the meantime, so snug them down and see how it goes - it’s a nice idea. Have you ever done the pancreas? I have. Can I have a hemostat? You’ve got to be careful - there’s a pancreas tear. So here’s my duct right here, right? Yeah, I’m going to go this way. Cuz I don’t want to “a” catch the duct, and “b” - there we go. Right through a vessel. Perfect. So I’m doing it as if I’m burying it.
Right now I’m doing a posterior wall for the duct - for the pancreatic duct - I'm not even doing the duck itself. I’m just pancreas to surosa of the - of the bowel. You know, if you do a two layer anastomosis. Yeah, I usually put four, but… Yeah, I’m using them slightly now because I want to see where the pancreatic duct actually is. Yep, that’s that one, that’s that one. That’s that one, that’s one. Right? So it looks like - let’s pull up a little bit on these. Pull up on those two, and I’ll pull on these. This thing came up. That works well. That looks pretty good. Alright, you have the debakey's? You guys stint these anastomoses? Yeah, I’m - I’m going to. Right there, you guys see the pancreatic duct? Yep, that’s what you got your pickups on right now, right? No, right there where Eric goes. Right there - right where that pickup is going. Do you see it? Okay. So I’m going to make my - yeah, something right here. Schmidt. Alright. Yeah, I do just to make sure I got - you’re actually sewing through it - the guy I trained with actually puts a chromic on it - so it pulls through? - all, all the way around so he knows he has it.
So let’s tie these. Okay. So tie this one. Do it gently so it doesn’t tear. Alright, leave that one on there. Hold this to the bowel. You can hold it for me like that - this way it’s not tearing away. Scissor. I’ll do the other inside, and then you do the last outside. It’s going okay. I got it, yep. Pull towards yours slightly. Yep.
We’ll adjust - these got to go up here now so they’re out of the way. I’m going to start using my loops here in a second. Looks okay. Stitch the - what do we got? 5-0 or 4-0 PBS? I’ll take a 5-0 PBS. Yeah, that’s me pulling it. We’ll need five of those please. We’ll try to put the suture in the duct - the needle in the duct - and then out versus the other way because then you can crack the mucosa or you might not get the mucosa. You know what I mean? Like I go in through like this which makes it more difficult at times.
Yeah. Suction. Hemostat. Scissor. So I’m small bowel round mucosa to - and then mucosa - and then out through - right. Do you take a bite of the small - the surosa - when you come out of the pancreas? On the - no, I didn’t want to.
Trying to do the posterior wall here. And then do this.
So I did the pan - the mucosa. Now I’m going to do the anterior layer. Do you have a 3-0 vicryl?
One layer for this one. Yeah. And then do one, two, three, four, five, and we’ll do anterior. We’ll probably need at least nine. Yeah, big bites - huge bites. You just gotta be careful cuz this artery, I bet you is back here, is dividing, going in there… So usually, I don’t make it this big. I know. Yeah, that’s what I was trying to do actually. That should be big enough. I’m just protecting our pancreas now. Suction. Why don’t you - why don’t you do a forehand to yourself? Come in here, right? Big bite. Bigger. Okay, good. Not too much mucosa, but that’s good. That’s alright. That’s fine, that’s good.
You get a good bite there? I can’t tell. You got a lot of mucosa. Yeah. You just need a little - just a little wisp. How much surosa did you get? That’s alright. Big huge bite - huge bite. Yeah. Alright, very good. So see mucosa there? And get a big bite of surosa. There you go. Yep, perfect. Perfecto. Suction, good, suction. Wa-a-a-ait. Did you get mucosa in there? There’s mucosa down there. Just - just take it. Let’s see. I don’t know yet. Pull up on it. Yeah, you got it, see? You have plenty.
So question is…
I don’t think that was anything to be honest with you. We have a stent going all the way through the main pancreatic duct. So... where am I? Over here. 45 min. 45 min too long. Just a little bit more. Okay. Alright, so hold that.
So what I like to do is after I do my anastomosis, I try and tack the stomach on the other side of that mesentery, so everything is below. You know what I mean? We’re going to do this posteriorly like that. And I’m going to tack - bring this stomach and we tack that posterior and you’ll see. Alright. Hold that. Where we’re making the enterostomy. We’re doing it on the posterior wall of the stomach. Alright, where we going? Which way does it go? We twisted now? Let’s see. Alright, so just hold it like this - that’s hold we want it.
So where are you going to make your enterotomy? Let’s go - you don’t have to be right at the mesentery. You know, you can actually have it like this and put it on this side a little bit, right? Cuz it will lie like this. Or you lay it like that and you put it over there - it doesn’t really matter. Yeah, it doesn’t matter. Make a small enterotomy there. It’ll go something like that there. Just go straight - yep. Schmidt. You in? Alright, give it a snip - the other way. Right there, looks good. Right where that vein is. Right where the anadral is. Open - all the way open - open, open. Alright, good. Stapler. Woah - like that. Push it in. Okay. No, open. Try not to open close - you know what I mean - abruptly. Slowly. Yep, alright, that’s better. I think that’s pretty good. Couple alysis and babcock. Any bleeding? Not really.
How do we want to do this? Like this or like this? Like this - I know, the food is going down the other way, so I think you could do it this way. Yeah. Doesn’t matter - whichever way you want to do it. Which way you want to do it? This way? I think it’s going to be harder to get the T in there. Yeah, I think it would be easy that way. Get the very corner - very, very corner, yeah. This one. Corner, corner, get the corner. Babcock. Think it gets through on that side okay. Hold the - hold one of these out for me. Like that. We got to bring that up higher. K - give it a close. Kinda like - go ahead, close. Keep closing. Okay. Yep, go ahead. Okay.
And now we narrowed this down - I like it the other way. Here we go, right? This is posterior wall. So now, I’ll lift this up, these two ends out, and go like this. Right? And then I tack this - there we go. So tack that there. Watch out for the vessel. Like here to here.
Pull, one more - one more in between. See the big hole? Here, yeah. Get away from the anastomosis. Yeah, I’m just closing the defect. No - well, we will be in about 5 min. Just where we did our - we did our gastrojejunostomy, we did a retrocolic, so the jejunum went underneath and through the mesentery so I’m just close and kinda yeah. Do you have a two? Do you have a Kocher? Let’s hold that over. Her ribs are here. So we got to go here. That suckers got to come all the way over there. Over the fascia, yeah. So let’s do something here I think. It’s going to be like right here. Let me see that. This is going to be as good as it's going to get for us. Do you have a Schmidt?
So you’re going to go from the other end, up - yep. So feel where her ribs are, look where the hole is. Make sure we have enough - make sure we have enough, you know - make sure we have enough fascia to close and we’re not right on her rib. There we - you can even come up here a little bit. Okay. You have scissors? Cut the - cut in between those two - no, no, no, no. That wouldn’t be good. So you take a little bit of that plastic that’s between them - like that, a little sliver - just a sliver. You don’t want to get underneath it cuz the tube’s there. Okay, good enough. Let’s go here. I don’t want to - well, our anastomosis is here. I can feel it. It’s right there. This way, we can just shove it. Yeah, and we have to make sure it goes that way.
So just - will - will this come over way over here without causing too much problems for our anastomosis - that’s the question. We have to do it eventually. Yeah, somewhere around there. Try for that vessel. Shove that in there. Okay, looks good. Hold onto that and I’ll tailwind. Okay, start to see if we can thread it through. Pull back just a hair. Okay. Go ahead, push it in again. Perfect. Perfecto. Keep going, get that thing in. It’s only when that - the balloon is past the - pass the stomach. Yeah, just get it in there. Alright, fill up your balloon. All ten. Make sure you’re not - take a feel where it’s pulling up. You’re doing it. Yep. Good. How’s it look? That’s as good as it gets. Right now. Yeah. How’s that? As good as - alright, good. Sometimes I do. Yeah this is a little tight, but it’s alright. I’d rather it be… I can still feel the stomach. I think that’s as good as it’s going to be though. I don’t think so, do you? See advantage of putting a drain in? Okay. Shove some of that like that. Alright.
CHAPTER 5
No, I don’t like Kochers, nah. Small rich. That’s through the knife blade - just make sure you know that, so don’t take it. Come over here. See if you come here - no, no, no, don’t cut here. This is where you go. Yep. Get a big bite, just don’t get her xiphoid. It’ll hurt.
Oh, I used to. You can tell the whipple patients just by the number of drains they have. Yeah, I just to put them in, but then the thought is maybe they increase your risk of having a leak or a - or if you do have a leak, it makes it worse because you’re sucking on it. So it’s just...
See - so can I see what's going on here? See we have more fascia on this side than on that side, right? See how close these sutures are compared to those sutures. So each time you go like this, you’re still creating the problem and makes it worse, so try and go straight across. Sorry. See that’s straight across, right? See how that’s straight across and it’s going to lie like that and we’re going to have a bigger gap. So now we just reverse it, and we still have a lot of fascia on your side. Just rev - yeah.
There we go. Alright. Thanks. I’ll dictate. Thank you. Thanks - good job.